In this issue of Blood, Sims et al1 describe clinical, genotypic, and phenotypic findings in 47 patients with the gray platelet syndrome (GPS), a rare recessive platelet disorder with α-granule abnormalities and mutations in NBEAL2. They expand the repertoire of granule defects in GPS to leukocytes and document an important association of GPS with immune dysregulation and autoimmune diseases.
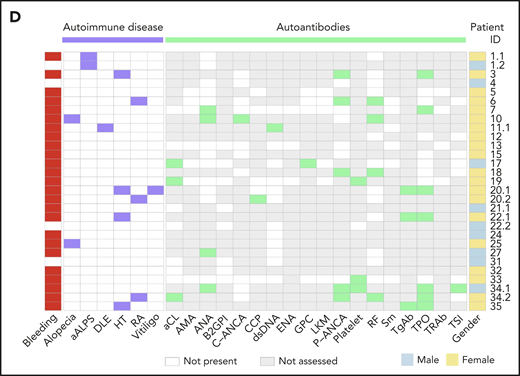
Spectrum of bleeding symptoms, results of autoantibody tests and autoimmune disease in 29 patients with GPS. See Figure 2D in the article by Sims et al that begins on page 1956.
Spectrum of bleeding symptoms, results of autoantibody tests and autoimmune disease in 29 patients with GPS. See Figure 2D in the article by Sims et al that begins on page 1956.
GPS is a heterogeneous bleeding disorder characterized by macrothrombocytopenia and selective deficiency of α granules and their contents. The name derives from the initial observation of gray appearance of platelets with a paucity of granules on blood films from a patient with a lifelong bleeding disorder. Other features include splenomegaly, myelofibrosis, and emperipolesis with neutrophils within megakaryocytes in the bone marrow. In 2011, 3 groups reported recessive variants in NBEAL2 as the cause for GPS.2 NBEAL2 is a BEACH-domain–containing protein linked to granule development. GPS has hitherto been considered essentially a platelet disorder. The current study, involving the largest cohort of 47 GPS patients studied to date, provides major insights on multiple aspects of GPS and NBEAL2.
From the perspective of the GPS disease, there are several findings, including the marked heterogeneity in NBEAL2 variants (70 etiological variants, 32 novel) and bleeding symptoms (5 patients had none), and the high prevalence of cytopenia of at least 1 leukocyte type (77% of patients), elevated B12 levels (91%), and bone marrow fibrosis (57%). Emperipolesis was noted in 58% of megakaryocytes in 3 GPS bone marrows studied (1% in controls). There was no association of granulocyte or monocyte cytopenia or of splenomegaly with BM fibrosis. There were no significant genotype-phenotype associations observed.
Selective platelet α-granule deficiency has been the hallmark of GPS. The current study extends the abnormalities associated with NBEAL2 mutations to multiple immune cells. The authors found decreased counts of neutrophils, monocytes, lymphocytes, eosinophils, and basophils in GPS patients and provide evidence of alteration in granules and their proteins.
Detailed studies document striking alterations in the transcriptome and proteome profiles in not only platelets but also neutrophils, monocytes, and CD4+ T cells and provide convincing evidence of a critical role for NBEAL2 in granule formation, spanning multiple blood cells. These findings implicating an effect on leukocytes are in line with studies in Nbeal2−/− mice.3,4 Of the differentially abundant proteins in platelets, neutrophils, and monocytes, Sims et al found that 89%, 86%, and 62%, respectively, were reduced in GPS patients, and they were enriched in granule proteins. Nine such proteins were reduced across at least 3 cell types. Interestingly, besides the expected decrease in α-granule proteins, GPS platelets had increased levels of 13 proteins, 5 of which are recognized neutrophil granule proteins, revealing platelet enrichment in neutrophil constituents.
A major finding in this study is the recognition of autoimmunity, autoantibody production, and inflammation in GPS patients, indicating the clinical consequences of the immune cell abnormalities. Autoimmune or infectious complications have been previously observed in a few GPS patients, and Nbeal2-deficient mice have increased susceptibility to infection or its complications.3,4 The current study identified an autoimmune disease diagnosis in 26% of GPS patients, including Hashimoto thyroiditis, rheumatoid arthritis, and atypical autoimmune lymphoproliferative syndrome (see figure). Mass spectrometry of plasma indicated an elevated acute phase response with increased C-reactive protein, reflecting ongoing inflammation.
At least 1 autoantibody was detected in more than half of the 29 GPS patients tested; antinuclear antibodies, antithyroid antibodies, and rheumatoid factors were among the most frequently detected autoantibodies (see figure). The authors found antineutrophil cytoplasmic antibodies (ANCAs) in a striking number of patients, out of 11 patients tested, 6 had a positive ANCA test, with a perinuclear ANCA (pANCA) pattern in 5 patients and a cytoplasmic ANCA (cANCA) pattern in 1 patient. This far exceeds the expected rate in routine hospital testing.5 Whether GPS patients develop small-vessel vasculitis, the classic clinical manifestation associated with ANCAs remains to be determined.
The presence of ANCAs in GPS patients raises an interesting possibility that altered granule processing predisposes to their development. Both pANCA and cANCA target neutrophil granule proteins: pANCAs and cANCAs typically bind myeloperoxidase and proteinase 3, respectively. Defective handling and clearance of myeloperoxidase has been reported to induce anti–myeloperoxidase antibodies and small-vessel vasculitis in murine models of drug-induced vasculitis6 ; thus, excess or aberrant availability of myeloperoxidase or other neutrophil granule proteins might help induce autoantibodies in GPS.
To add to the intrigue, proteomic analyses revealed that GPS platelets contain increased myeloperoxidase and other neutrophil proteins. How do neutrophil proteins express themselves in circulating platelets? Endocytosis comes to mind, and platelets are avid imbibers. However, it is tempting to speculate, as the authors do, that it may be related to impressive emperipolesis observed. Emperipolesis induces transfer of neutrophil membranes to the platelet progeny and impacts platelet production.7 Because of a pancellular defective handling of granule proteins, the engulfed neutrophil may transfer proteins into the megakaryocyte milieu and to platelet progeny more easily and may promote antibody development.
CD4+ T-helper cells are strongly associated with development of multiple autoimmune conditions.8 Unlike monocytes and neutrophils, CD4+ T cells from GPS patients contained increased levels of multiple proteins, accompanied by increased gene expression, suggesting that the total pool contains more activated or memory T cells. It will be of interest to immunophenotype T-cell populations in GPS patients to determine the frequencies of effector/memory T-cells subsets, including subsets associated with autoantibody production, such as T-follicular helper cells and T peripheral helper cells.9,10 Also of interest are the phenotypes and functions of CD8+ T cells and natural killer cells, which rely more heavily on granules for their function and show functional defects in Nbeal2-deficient mice.3
The wealth of findings from this large study paints a novel landscape of GPS, that it is more than a platelet disorder, indeed, a systemic disorder encompassing leukopenia, autoimmune disorders and antibodies, inflammation, and infection. They expand the role of NBEAL2 in a major way, showing that it regulates formation and function of granules across multiple hematopoietic cells.
Conflict-of-Interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal