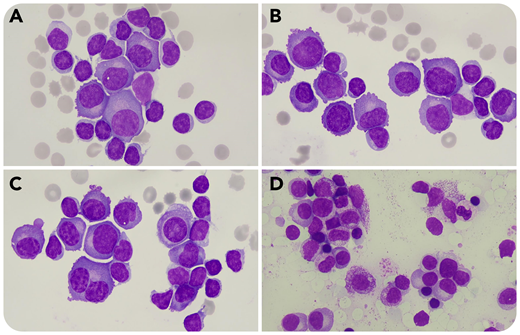
A 79-year-old woman presented with asthenia, anorexia, weight loss, and low back pain. Chest radiograph showed a moderate bilateral pleural effusion (PE). Analysis of pleural fluid showed 2623 × 106 nucleated cells per L, 3002 × 106 erythrocytes per L, protein concentration of 50.2 g/L, and negative microbiological tests. Microscopic observation of a cytocentrifuged sample revealed 74% lymphocytes and the presence of 26% medium-to-large size atypical cells with round eccentric nuclei (some cells were binucleated) and basophilic cytoplasm compatible with atypical plasma cells (PCs) (panels A-C: pleural fluid; 100× objective; May-Grünwald-Giemsa stain; original magnification ×1000). These cells were CD138 positive by flow cytometry, confirming the presence of PCs in the PE. Capillary electrophoresis and immunofixation in serum demonstrated monoclonal immunoglobulin G (IgG) λ and free λ chains. Bone marrow (BM) aspirate contained 25% PCs (panel D: BM; 50× objective; May-Grünwald-Giemsa stain; original magnification ×500), IgH rearrangement, and translocation (11;14). Computed axial tomography showed posterior paravertebral mediastinal tumor, which is suggestive of plasmocytoma. The patient was finally diagnosed with IgG λ multiple myeloma (MM).
MM represents abnormal proliferation of neoplastic PCs and is one of the most common hematologic malignancies affecting BM. About 6% of patients with MM develop PE, mainly nonmyelomatous. Myelomatous pleural effusion (MPE) resulting from PC infiltration is rare and has an incidence of ∼1%. It is crucial to screen patients with MM who have PE for MPE because it indicates a poor prognosis.
A 79-year-old woman presented with asthenia, anorexia, weight loss, and low back pain. Chest radiograph showed a moderate bilateral pleural effusion (PE). Analysis of pleural fluid showed 2623 × 106 nucleated cells per L, 3002 × 106 erythrocytes per L, protein concentration of 50.2 g/L, and negative microbiological tests. Microscopic observation of a cytocentrifuged sample revealed 74% lymphocytes and the presence of 26% medium-to-large size atypical cells with round eccentric nuclei (some cells were binucleated) and basophilic cytoplasm compatible with atypical plasma cells (PCs) (panels A-C: pleural fluid; 100× objective; May-Grünwald-Giemsa stain; original magnification ×1000). These cells were CD138 positive by flow cytometry, confirming the presence of PCs in the PE. Capillary electrophoresis and immunofixation in serum demonstrated monoclonal immunoglobulin G (IgG) λ and free λ chains. Bone marrow (BM) aspirate contained 25% PCs (panel D: BM; 50× objective; May-Grünwald-Giemsa stain; original magnification ×500), IgH rearrangement, and translocation (11;14). Computed axial tomography showed posterior paravertebral mediastinal tumor, which is suggestive of plasmocytoma. The patient was finally diagnosed with IgG λ multiple myeloma (MM).
MM represents abnormal proliferation of neoplastic PCs and is one of the most common hematologic malignancies affecting BM. About 6% of patients with MM develop PE, mainly nonmyelomatous. Myelomatous pleural effusion (MPE) resulting from PC infiltration is rare and has an incidence of ∼1%. It is crucial to screen patients with MM who have PE for MPE because it indicates a poor prognosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal