
Background: Sickle cell disease (SCD) is a genetic hematologic condition affecting more than 300,000 individuals worldwide. Most of the 100,000 individuals with SCD in the United States are African-American. An estimated 50% of those with the most severe genotype of SCD (HbSS) will have an overt or silent cerebral infarct (SCI) by age 30. While a significant number of studies have addressed the cognitive function and brain imaging of children with SCD, very few have included adults. As disease modification has increased over the last decade, a modern assessment of adults with SCD is needed.
The aims of this study are to:
1. Determine the prevalence of cognitive impairment in adults with SCD
2. Determine if adults with SCD have deficits in functional task performance skills
3. Assess if and how cognitive function and task performance change over time
Methods: This is a cross-sectional analysis of a prospective, observational cohort study. Adults, 18 years of age or older, with any form of SCD were recruited from the SCD clinics at Washington University in St. Louis. During baseline testing, participants completed the Wechsler Abbreviated Scale of Intelligence (WASI-II), National Institutes of Health Toolbox Cognition Battery (NIHTB-CB), and the Medication subtest of the Executive Function Performance Test (EFPT-M). The WASI-II and NIHTB-CB were repeated annually. Mean participant data from the baseline WASI-II and NIHTB-CB were compared with normative individual measure and composite scores using a one-sample t-test. The NIHTB-CB normative mean is a t-score of 50 with a SD of 10. Baseline results on Medication subtest of the EFPT were compared to previously tested control and stroke groups. Higher scores on the EFPT are indicative of greater executive dysfunction. Differences between Time 1 and Time 2 scores were evaluated using a paired-samples t-test. Univariate analyses were used to describe relationships between cognition and patient factors. Annual magnetic resonance imaging (MRI) was also conducted to assess infarct classification, with completion limited to 12-18 months from consent. Radiographical analyses were reviewed and recorded by the study neuroradiologists.
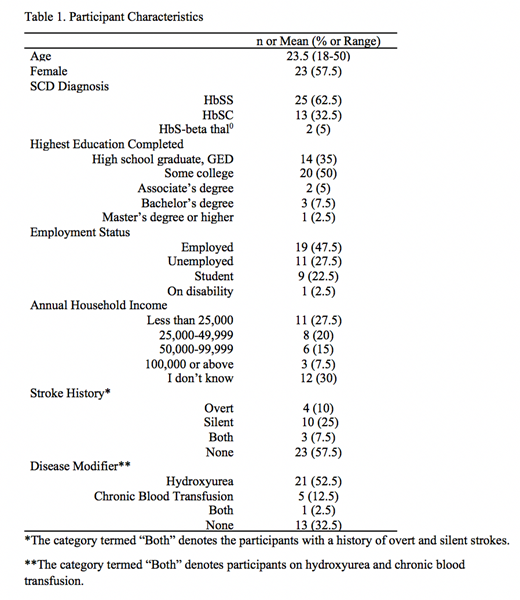
Results: Forty participants were assessed at baseline; 9 completed Time 2 testing. Participant demographic information is presented in Table 1. Compared to the normative population, no significant differences were found on the WASI-II. On the NIHTB-CB, participants scored significantly lower on subtests measuring processing speed (Mean difference -13.8, p <.001), executive function (Mean difference -8.93, p = .001), attention (Mean difference -13.15, p < .001), working memory (Mean difference -5.68, p = .001), overall fluid cognition (Mean difference -13.08, p < .001), and total cognition (Mean difference -5.87, p = .002). Participants scored significantly higher than previously tested control (Mean difference 1.68,p <.001) and mild-stroke groups (Mean difference 1.18, p < .001) on the EFPT-M. Deficits in self-awareness were noted on all performance-based measures. No significant differences were found between participant means on Time 1 vs. Time 2 testing (Mean = 1.02 years, Range =.97-1.12). Participants with more severe phenotypes of SCD (HbSS or HbS-beta thal0) performed lower on the NIHTB test of attention when compared to those with HbSC (Mean difference -6.26, p=.039). History of stroke or use of disease modifiers had no relationship with cognitive outcomes.
Of the 59 participants consented to yearly MRI evaluation, 45 have completed baseline imaging and 1 completed Time 2 imaging. Radiographical impressions reported: 1) overt strokes in 2 participants on transfusions (TF), 1 on hydroxyurea (HU), and 1 on no disease-modifying regimen (ND); 2) SCIs in 6 participants on TF, 6 on HU, and 4 on ND; 3) no infarct in 1 participant on TF, 18 on HU, and 9 on ND.
Conclusion: Adults with SCD in this relatively highly educated cohort have marked deficits in executive function, attention, working memory, processing speed, and self-awareness. Cognitive deficits lead to difficulty completing everyday functional and disease-related activities, ranging from medication adherence to productivity in education and employment. Healthcare providers who treat individuals with SCD should be aware of the cognitive impairments in this population. Routine cognitive screening is needed to initiate referrals for cognitive rehabilitation.
King:Magenta Therapeutics: Membership on an entity's Board of Directors or advisory committees; Novimmune: Research Funding; RiverVest: Consultancy; Tioma Therapeutics (formerly Vasculox, Inc.):: Consultancy; WUGEN: Equity Ownership; Incyte: Consultancy; Amphivena Therapeutics: Research Funding; Cell Works: Consultancy; Bioline: Consultancy; Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal