
Introduction: For warfarin-treated patients with atrial fibrillation (AF) or venous thromboembolism (VTE), concomitant use of aspirin and warfarin increases the risk of major bleeding 1.5-1.8 fold without an apparent reduction in thrombotic events when there is no clear indication for combination therapy. As a result, each of six anticoagulation clinics in the Michigan Anticoagulation Quality Improvement Initiative (MAQI2) consortium implemented a common intervention between late 2017 and mid 2018 aiming to reduce inappropriate aspirin use. The intervention consisted of a screening process to identify possible inappropriate aspirin use and then contacting the patient's provider to discuss the need for ongoing aspirin therapy. Site-level implementation variation included the personnel carrying out the intervention, the use of technology, and the means of provider communication. Treatment decisions were deferred to the treating provider but facilitated by the anticoagulation clinic staff.
We sought to assess the impact of this intervention on the rate of inappropriate aspirin use over time and compare patient characteristics based on aspirin use post intervention.
Methods: First, we compared the overall rate of inappropriate aspirin use among the six center MAQI2 anticoagulation clinic cohort immediately before and after the intervention. All patients in MAQI2 were treated with warfarin. Then, we identified a sub-cohort of warfarin-treated patients with AF and/or VTE enrolled between January 2010 to June 2019. Within that sub-cohort, we assessed aspirin use pre and post the site-specific date of implementation of the intervention. Patients with a potential indication for aspirin use were excluded (e.g., any history of coronary artery disease, myocardial infarction, percutaneous coronary intervention, mechanical heart valve replacement, left ventricular assist device placement, peripheral arterial disease, or coronary artery bypass grafting). Each site was able to further restrict who was targeted for intervention (for example, excluding patients with a history of antiphospholipid syndrome or stroke).
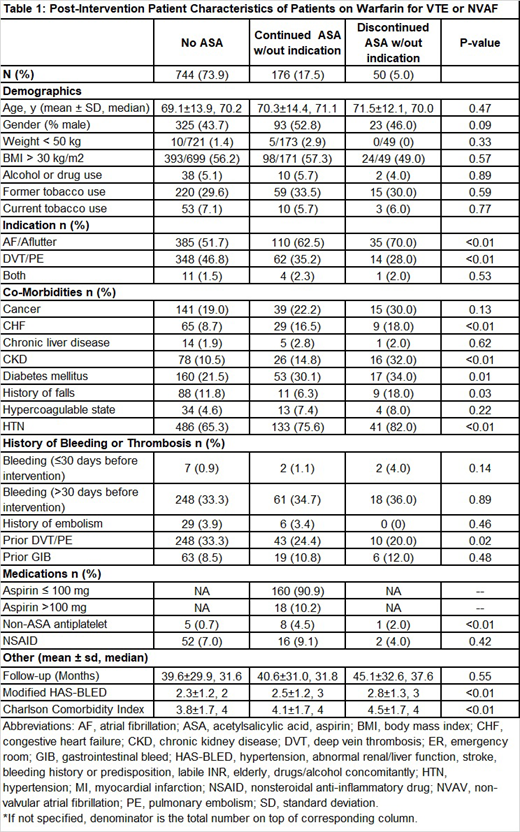
Using site specific definitions for inappropriate aspirin use we identified four groups at the end of the study period: 1) patients not on aspirin, 2) aspirin-using patients without an apparent indication who stopped aspirin following implementation, 3) aspirin-using patients without an apparent indication who remained on aspirin following implementation, and 4) aspirin-using patients who developed an indication for aspirin during the study period. To assess inappropriate aspirin use in our cohort, the characteristics of the first three groups were compared.
Results:
Between August 2017 and May 2019, a total of 3,766 warfarin-treated patients enrolled in MAQI2. Following implementation, inappropriate aspirin use was reduced by 34% (from 27.9% [401/1437] to 18.5% [251/1356]). A sub-cohort of 1,007 patients who met the inclusion criteria had clinical follow-up pre and post intervention and were followed for an average of 40.1 months from enrollment to their first follow-up post-intervention. Of this sub-cohort, 226 (22.4%) were inappropriately on aspirin, with 50 (22.1%) stopping aspirin. A small number of patients 37 (3.7%) developed an indication for aspirin (e.g., myocardial infarction) during the study period and were removed from this analysis.
As compared to patients not taking aspirin, patients on inappropriate aspirin were more often taking warfarin for AF, had congestive heart failure, chronic kidney disease, diabetes mellitus, hypertension, and had a higher Charlson Comorbidity index; they were less likely to have VTE or a history of VTE. As compared to patients continuing on aspirin following implementation, patients stopping inappropriate aspirin were more likely to have chronic kidney disease (p=0.02) or a history of falls (p=0.03).
Conclusion:
Among warfarin-treated patients with AF or VTE, inappropriate aspirin usage can be identified and significantly reduced using a simple intervention in the anticoagulation clinic. Patients at higher risk of bleeding may be more likely to have their aspirin discontinued. Further studies are needed to see if reducing inappropriate aspirin usage translates to improved clinical outcomes and to determine the reasons for patient persistence on inappropriate aspirin.
Kaatz:Janssen: Honoraria, Research Funding; Pfizer: Honoraria; Bristol Myers Squibb: Honoraria; Portola: Honoraria. Kline-Rogers:AC Forum: Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria; QUANTUM-AF: Membership on an entity's Board of Directors or advisory committees. Sood:Bayer: Research Funding. Froehlich:Blue Cross Blue Shield of Michigan: Research Funding; Novartis: Honoraria; Boehringer-Ingelheim: Honoraria; Fibromuscular Dysplasia Society: Research Funding; Merck: Honoraria; Pfizer: Honoraria; Janssen: Honoraria. Barnes:Portola: Honoraria; Pfizer/Bristol Myers Squib: Research Funding; Pfizer: Honoraria; AMAG Pharmaceuticals: Honoraria; Bristol Myers Squib: Honoraria; Blue Cross Blue Shield of Michigan: Research Funding; Janssen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal