Background. High rates of response and minimal residual disease (MRD) negativity have been reported with the use of novel treatment options in multiple myeloma (MM) patients (pts) eligible for autologous stem-cell transplantation (ASCT). Despite very promising results, there is still a proportion of pts who do not respond to therapy or relapse early. This represents an unmet medical need.
Aim. To identify the main factors predictive of early relapse in the context of novel treatment approaches.
Methods. Data from newly diagnosed MM (NDMM) pts ≤65 years enrolled in the FORTE trial were analyzed. The evaluated baseline standard clinical and biological features included: age, Hb, creatinine, tumor circulating plasma cells (PCpb) evaluated by flow cytometry, bone marrow plasma cells (PCbm) evaluated as continuous variables, free light chain (L vs K), M-component subtype (IgA vs others), Revised International Staging System (R-ISS II/III vs I), LDH (>ULN vs ≤ULN), ISS (III vs II vs I), presence vs absence of chromosomal abnormalities detected by FISH [(del17p, t(4;14), t(14;16), t(11;14), amp1q, del1p, del13], and presence vs absence of plasmacytomas. Pts were randomized to receive carfilzomib, lenalidomide, dexamethasone (KRd) induction - ASCT intensification - KRd consolidation (arm A); KRd12 (arm B); and carfilzomib, cyclophosphamide, dexamethasone (KCd) induction - ASCT intensification - KCd consolidation (arm C). Thereafter, patients were randomized to maintenance with lenalidomide alone or lenalidomide plus carfilzomib. Pre-maintenance MRD evaluation was performed by 8-color second generation flow cytometry (sensitivity 10-5) in patients who achieved at least a very good partial response (VGPR). Early relapse was defined as relapse ≤18 months from randomization. Univariate feature selection was performed between both categorical and continuous baseline variables and the achievement of pre-maintenance MRD negativity, according to Chi-square and Kruskal tests. The same baseline features, plus the achievement of MRD negativity, were included in a univariate analysis to select candidate predictors of early relapse. Selected features were then included in a multivariate logistic model. A multivariate analysis was performed to evaluate predictors of MRD negativity and early relapse. The model was adjusted for age and administered therapy.
Results. 474 patients were enrolled in the trial. Baseline features were well balanced in the 3 arms.
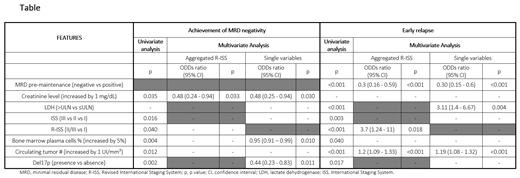
Predictors of MRD negativity (10-5): In univariate analysis, the baseline factors selected basing on the probability of achieving pre-maintenance MRD negativity were creatinine levels, ISS stage, R-ISS stage, del17p, PCbm (P=0.004) and PCpb. In multivariate analysis, including single variables not aggregated in R-ISS, increased creatinine levels (OR 0.48, 95% CI 0.25-0.94, P=0.03), increased PCbm (OR 0.95, 95% CI 0.91-0.99, P=0.01) and presence of del17p (OR 0.44, 95% CI 0.23-0.83, P=0.01) reduced the probability of achieving MRD negativity (Table).
Predictors of early relapse: In univariate analysis, the main baseline factors selected basing on the risk of early relapse were LDH, ISS, R-ISS, PCbm, PCpb, del17p and achievement of MRD negativity. In multivariate analysis, R-ISS II/III vs I (OR 3.7, 95% CI 1.24-11, P<0.001) and PCpb (OR 1.2, 95% CI 1.09-1.33, P<0.001) significantly increased the risk of early relapse, while the achievement of MRD negativity significantly decreased the risk of early relapse (OR 0.3, 95% CI 0.16-0.59, P<0.001). When multivariate analysis was performed including LDH, ISS and chromosomal abnormalities instead of R-ISS, both PCpb and MRD maintained their significant impact; moreover, high LDH level was the variable in the R-ISS that determined an increased risk of early relapse (OR 3.11, 95% CI 1.40-6.67, P=0.003).
Discussion. In the context of novel highly effective treatment approaches, creatinine levels, PCbm and, in particular, presence of del17p reduced the probability of achieving MRD negativity. Multivariate analysis combining baseline features and MRD negativity highlights how comprehensive baseline evaluation including baseline R-ISS (or in particular high LDH levels, which may have an independent role) and circulating PC can help to identify patients at high risk of early relapse. However, the achievement of MRD negativity is the factor that may reduce the risk of early relapse.
Gay:Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees. Offidani:Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees. Vozella:Celgene: Honoraria; Amgen: Honoraria. Belotti:Janssen: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees. Galli:Takeda: Honoraria; Leadiant (Sigma-Tau): Honoraria; Janssen: Honoraria; Celgene: Honoraria; Bristol-Myers Squibb: Honoraria. Gozzetti:Celgene: Honoraria; Amgen: Honoraria; Jansenn: Honoraria; BMS: Honoraria. Giuliani:Janssen: Research Funding. Musto:Amgen: Honoraria; Celgene: Honoraria. Cavo:sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; novartis: Honoraria; takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel accommodations, Speakers Bureau; janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel accommodations, Speakers Bureau; bms: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Boccadoro:Sanofi: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; AbbVie: Honoraria; Mundipharma: Research Funding.
The presentation includes discussion of off-label use of a drug or drugs for the treatment of multiple myeloma.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal