Background:
Sickle cell disease (SCD) is the most common hereditary red blood cell disorder in the United States (USA) and primarily affects African-Americans. Of the four most common sickle cell genotypes, SS and Sβ0 are associated with greater severity, including more ischemia due to sickling and more profound microvascular changes from chronic sickling, as compared to those with the Sβ+ and SC genotypes. African-Americans suffer from high rates of Type 2 Diabetes mellitus (T2DM), a disease associated with deleterious microvascular changes when blood glucose is poorly controlled. Recent epidemiologic studies suggest the prevalence of T2DM among African-Americans with and without SCD in the USA are similar around 15-20% and that patients with SCD and T2DM are more likely to be overweight than those without T2DM (Zhou etal., Br J Haematol, 2019). However, the prevalence of diabetes among the different genotypes of SCD remains unknown (Skinner etal., Br J Haematol, 2019). Furthermore, the HbA1C, which is often used to screen, diagnose and monitor long-term control of T2DM in patients is not reliable in patients with SCD and data suggests that fructosamine may be a more reliable marker in this patient population (Smaldone, 2008). If SCD patients with T2DM are undiagnosed or undertreated, they may develop preventable complications related to their vasculopathy. In this study, we assessed both the prevalence of T2DM among adults with various SCD genotypes at our institution and the methods of monitoring long-term control among these patients.
Methods:
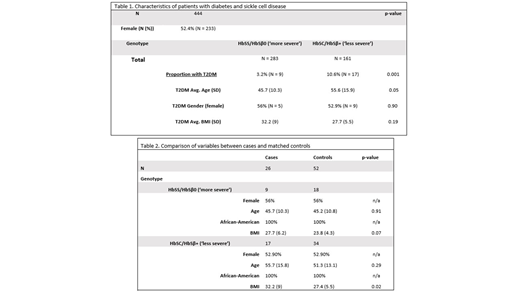
The University of North Carolina (UNC) Sickle Cell Database was used to conduct a single- institution, retrospective cross-sectional study of sickle cell patients and matched controls. A query of electronic medical records identified adult patients > 18 years old with both SCD (SC, Sβ+, SS, or Sβ0) and T2DM seen in the UNC Hospital system in the past 5 years Age, race, gender, BMI, and the frequency of fructosamine and HbA1C values were evaluated. Patients were divided into 2 groups - less severe (SC/Sβ+) vs. more severe (SS/Sβ0). Controls without T2DM were randomly selected from the database and matched 2:1 to cases based on SCD genotype, age, race, and gender for body mass index (BMI) comparisons. Unadjusted statistical tests were used to examine how the group with the more severe SCD genotype (SS/Sβ0) differed from the less severe genotype group (SC/Sβ+) based on T2DM diagnosis and BMI.
Results:
We identified 444 adult patients with SS, Sβ0, SC, or Sβ+ - 283 patients with more severe SCD (SS/Sβ0) and 161 patients with less severe SCD (SC/Sβ+). Twenty-six patients had a co-diagnosis of T2DM; all identified as African-American (see Table 1). A significantly higher proportion of the less severe SCD group were diagnosed with T2DM as compared to the more severe group (χ2 =10.13, p = 0.001). A higher proportion of patients diagnosed with T2DM and SCD had a BMI of 25kg/m2 (i.e. overweight) or greater (76.9%) compared to matched controls (59.6%, χ2 = 2.29, p = 0.13) (see Table 2). Of the patients diagnosed with SCD and T2DM within our database, 81% had an HbA1C resulted in the EMR within the past 5 years and 62% had a fructosamine resulted during the same time period; in the past 6 months 31% had an HbA1C resulted and 19% of patients had a fructosamine resulted.
Conclusion:
Patients in the less severe SCD group were more likely to be diagnosed with T2DM in our cohort as compared to the more severe genotype group. Notably, the T2DM prevalence for both the severe group (10.6%) and less severe group (3.2%) was lower than that reported by Zhou et al., 2019, suggesting under diagnosis of T2DM among adults with SCD. Our findings also suggest patients with SCD who are overweight or obese may be at risk for T2DM. Variability in the monitoring of T2DM among SCD patients was evident by the ordering patterns of fructosamine and HbA1C. Hematologists treating patients with SCD should be aware of the inaccuracy of HbA1C in this patient population and ensure patients with SCD and T2DM are monitored appropriately. Further investigation is needed to determine if our findings are applicable to larger cohorts.
Little:Hemex Health, Inc.: Patents & Royalties; GBT: Research Funding. Carden:GBT: Honoraria; NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal