Introduction:
Sickle Cell Disease (SCD) is a chronic, congenital hemoglobinopathy characterized by progressive multiorgan dysfunction (Vichinsky, ASH proceedings). The brain is one of the major organs affected by SCD. While it is known that neurocognitive defects can be seen even in the absence of overt stroke and silent cerebral infarcts, there are no specific guidelines for performing neurocognitive assessments on patients with SCD. We report our findings in 20 patients that received neurocognitive testing at our institution within the last 3 years
Methods:
Eligible participants were identified through the Chicago Sickle Cell Disease Research Group (CSCDRG) Registry in conjunction with the SCD medical team and pediatric psychologist. Enrolled subjects took part in child/caregiver interviews, caregiver questionnaires, and review of relevant medical and school records. Participants and caregivers completed a baseline neuropsychological evaluation, which included the Wechsler Intelligence Scale for Children (WISC). Questionnaires were also sent to participants' teachers. Medical chart review was used to collect information about genotype and relevant imaging.
Results:
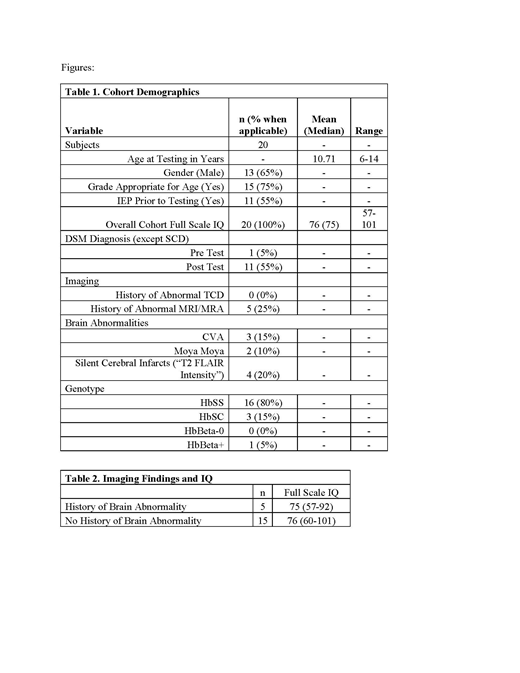
Neurocognitive testing was performed on 20 pediatric patients ranging in age from 6 to 14 years of age. The majority of patients had sickle cell genotype Hgb SS (n=16, 80%). Five patients (25%) had an abnormal MRI prior to testing. Brain abnormalities included CVA (n=2), Moya Moya (n=2), and T2 signal intensity (n=4). Cohort average full scale IQ was 75. Average full-scale IQ scores did not differ between patients who had a known brain abnormality (75) and patients who did not have a known brain abnormality (76) prior to testing. Most of the patients (n=15, 75%) were in the grade appropriate for age but only about half of the patients had an Individualized Education Plan (IEP) at the school. Interestingly, we also found that prior to neurocognitive testing, only one patient had a known Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5) diagnosis. Following testing, we identified ten additional patients who met criteria for at least one DSM-5 diagnosis. DSM-5 diagnoses in pediatric patients fell under primarily three categories including Neurodevelopmental Disorders (i.e., Attention-Deficit Hyperactivity Disorder, Specific Learning Disability in Mathematics), Trauma and Stressor Related Disorders (i.e., Adjustment Disorder with depressed mood), and Disruptive, Impulse Control and Conduct Disorders (i.e., Oppositional Defiant Disorder).
Conclusion:
We have described the differences in a pediatric sickle cell patient population who underwent neurocognitive testing. Our cohort of children with sickle cell disease exhibit significant neurocognitive deficits even in the absence of overt imaging findings or clinical stroke. Our findings also suggest that patients with SCD are at a higher risk of clinically significant mental health disorders which, if left undiagnosed, have the potential to hinder scholastic and occupational achievement. Individualized educational plans and specific interventions and addressing learning disabilities will help improve academic performance. Furthermore, neurocognitive testing should be a part of routine evaluation in patients with sickle cell disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal