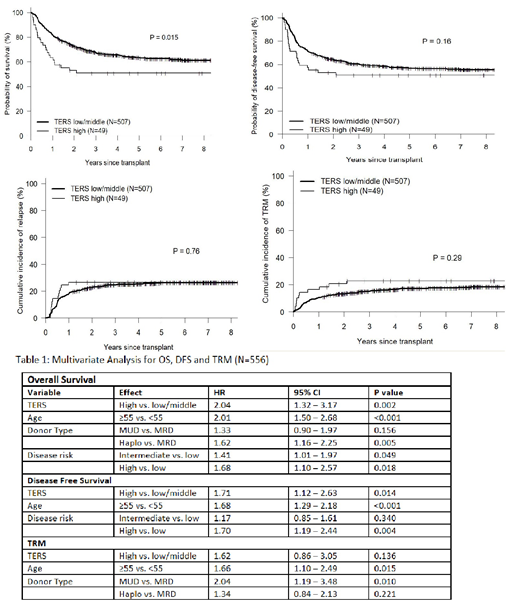
Psychological and social factors are utilized as important part of the evaluation process for patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT). The integration of such factors into the selection of suitable candidates and predicting survival post HSCT is still not widely incorporated in HSCT as it is the case in solid organ transplantation. To evaluate the impact of psycho social risks on post HSCT outcomes such as overall survival (OS), transplant related mortality (TRM), disease free survival (DFS), relapse and length of hospital stay, we prospectively conducted psycho social assessment on 556 consecutive allogeneic HSCT recipients who received their first transplant at our center between 2005 and 2017. The Transplant evaluation rating scale (TERS) has been previously published and was found to be psychometrically sound within the HSCT population(Hoodin, F. and Kalbfleisch, KR., Journal of Psychosomatic Research, 2003.) . TERS score was prospectively assessed by a psychologist prior to transplantation and patients were labeled as low/intermediate risk versus high risk based on their TERS score. All patients were transplanted in the outpatient setting with admission to the inpatient unit if clinically warranted. Five hundred and seven low/intermediate TERS patients and 49 high TERS were included in the analysis. Patients in the low/intermediate risk TERS group were more likely to have a higher disease risk index (17% versus 10%, p<0.001) and more likely to be transplanted in recent years (35% in 2015-207 versus 20% for high risk; p 0.005). Patients in high TERS group had longer, yet not significant, hospital stay during the first 180 days post allogeneic HSCT ( 21 vs 14 days for low/intermediate TERS p=0.22). Both groups had similar median age, sex, disease distribution, donor type, graft source, regimen intensity, HCT-CI score and KPS score. Median follow up for survivors was 66.7 months (14.0-184.4) for low/intermediate risk versus 94.8 months (15.9-182) for high TERS p<0.001. The survival estimates for low/intermediate and high TERS at 1 year were as follows (figure 1): OS (82% vs 63%, p=0.015), DFS (72% vs 57%), TRM (10% vs 16%) and relapse (18% vs 27%). The cumulative incidence of grade 2-4 GVHD and moderate-severe chronic GVHD were 38% and 30% for low/intermediate versus 31% and 27% for high TERS (P=NS). A multivariate analysis using cox models for OS, DFS, TRM, relapse , acute and chronic GVHD was performed using the following variables that were selected based on significance (p<0.05): age (<55 vs ≥55 years), gender, diagnosis, donor type (MRD, MUD, Haplo), source (BM, PBSC), regimen intensity, disease risk (low, intermediate, high), HCT-CI (0-2, ≥3), KPS (60-80, >80) and year of transplant ( 2005-2009, 2010-2014, 2015-2017). High TERS score predicted for worse OS (HR 2.04; 95% CI 1.32-3.17; p=0.002), worse DFS (HR 1.71, 95% CI 1.12-2.63, p0.014), a trend towards higher TRM (HR 1.62, 95% CI 0.86-3.05, p0.136) and relapse (HR 1.56, 95% CI 0.87-2.78, p=0.132) (table 1). In a subset analysis of patients with low/intermediate disease risk, multivariate analysis showed that high TERS predicted for worse OS (HR 1.97, 95% CI1.24-3.14, p=0.004), DFS (HR 1.74, 95% CI 1.10-2.75, p=0.018), trend for higher TRM (HR 1.91, 95% CI 0.98-3.72, p=0.057) and similar relapse rates. 1-year OS and DFS were significantly better for low/intermediate TERS 83% and 75% compared to high TERS 63% and 55% (p<0.05 for both) for patients with low/intermediate disease risk. Among a subset of patients with low HCT-CI ≤2 (n=317), patients in the high TERS group had higher TRM (25% vs 7%, p0.009) but no significant difference in OS, DFS, relapse and GVHD rates. In a multivariate analysis for HCT-CI 0-2 patients, high TERS was significant for higher TRM (HR 2.17, 95% CI 1.45-6.97, p=0.004). Our findings show that psycho social factors as measured by TERS score are a strong predictor of morbidity and mortality after allogeneic HSCT. This effect is independent of disease risk and morbidity prior to transplant. Psycho social factors should be included in patient selection and survival prediction models for transplant recipients.
Figure 1: Survival and Relapse Estimates Based on TERS score
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal