RS and AE, and OK and AN, had an equal contribution
Background: Oral mucositis (OM) is a debilitating complication of allogeneic hematopoietic stem cell transplantation (HSCT) propagated by an inflammatory response. While certain patient and transplantation-related characteristics increase the risk of OM, there is marked variability in OM severity across recipients even of the same treatments. Given the substantial perturbation of the gut microbiome following transplantation and its role in facilitating immune and metabolic functions, we hypothesized that the oral microbiome is also disturbed during transplantation and may explain population variation in OM severity.
Methods: In this single-center observational study, we prospectively collected weakly saliva samples from adult patients undergoing allogeneic HSCT and 20 healthy control volunteers. A total of 625 saliva specimens were collected starting from 7 days before HSCT to 34 days post-transplant. Patients gave a median of 4 samples (range 1-7). Samples underwent 16S rRNA gene sequencing (V4 region) on the Illumina platform. Pre-transplantation samples were defined as those collected between days -7 and -1. Sixty pre- and post-HSCT samples underwent mass spectrometry-based metabolomic profiling (Metabolon, Durham, NC).
For all patients, OM was graded according to the Common Terminology Criteria for Adverse Events (CTCAE) v4.0, with grade 3-4 defined as severe mucositis.
Results: In this largest analysis of the oral microbiome in transplant recipients, 184 patients were included. Transplantation indications varied, the leading being AML (47%). Myeloablative conditioning regimens were used in 70% of patients. Methotrexate (MTX) was given as graft-versus-host disease prophylaxis in 74% of patients. Median time to OM development was 7 days (IQR 5-9); 58% and 43% of patients developed grade 2-4 and grade 3-4 OM, respectively.
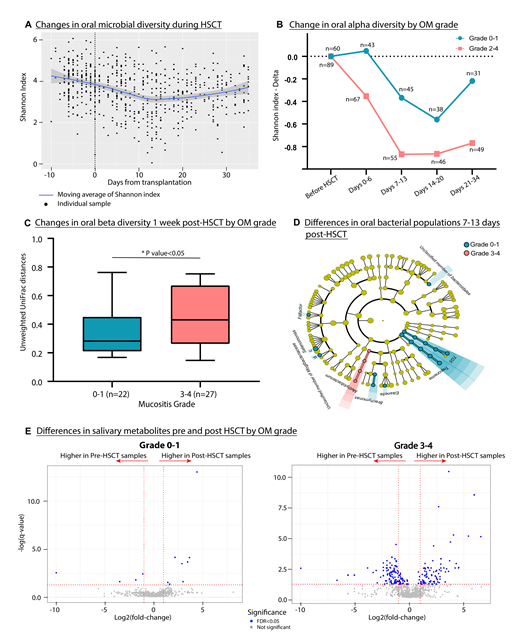
Pre-transplantation oral α-diversity, as measured by the Shannon Index, was similar to that of healthy controls (p=0.460), but later decreased, reaching a trough on day 12 followed by an increase to levels that were lower than baseline at day 34 (Fig. 1A). Indeed, there was a 24% reduction in peri-engraftment α-diversity relative to pre-transplant (p<0.001). Among patients with grade 2-4 OM, the reduction in α-diversity over time was more pronounced compared to transplant-recipients had no or only mild OM (grade 0-1) (Fig. 1B).
Since MTX is an established risk factor for OM and is known to induce microbiota alterations in the gut, we restricted the analysis hereon to the 135 patients exposed to MTX. Interestingly, using linear discriminant analysis effect size (LEfSe), Rothia, Kingella, and Atopobium were enriched in pre-transplant samples of patients who went on to develop severe OM. In a pair-wise analysis of samples collected on days -7 to -1 and 7 to 13, the decrease of α-diversity and increase in β-diversity was more pronounced in patients with grade 3-4 OM compared to those with 0-1 OM (Fig. 1C). In samples collected between days 7 to 13, saliva communities of patients with severe mucositis were more likely to harbor Methylobacterium while those in patients with grade 0-1 had a higher abundance of Treponema and the genus TG5 (Fig. 1D). Finally, metabolic profiling of saliva collected pre and post HSCT showed marked changes before and after transplantation in patients developing mucositis (Figure 1E). Microbiome-associated metabolites enriched in patients developing mucositis included histidine, phenylalanine, tyrosine, and tryptophan.
Conclusions: We demonstrate that the oral microbiota is disrupted during allogeneic HSCT. Microbiota injury is more profound in patients who developed oral mucositis. Our findings indicate that there may be a distinct microbiological and metabolic signature in patients with mucositis, with some changes preceding the clinical phenotype. These may serve as potential intervention points to treat and prevent mucositis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal