Background: Multiple Myeloma (MM) is a rare hematologic malignancy estimated to account for 1.8% of all new cancer cases in 2018. Although there are many studies evaluating the risk of second malignancies following MM, very few data is available regarding the risk of secondary smoldering myeloma (SM) and symptomatic MM (i.e., after receiving chemotherapy or radiation therapy for other types of cancer). The previous cytotoxic therapy has potential to cause or modify the myelomagensis process. Hence, to delineate clinical characteristics and biological behavior of secondary disease we analyzed the data in National Cancer Database (NCDB) which covers more than 70% of cancer patients (pts) in United States.
Methods: We reviewed pts in the NCDB who were diagnosed with MM between 2004 and 2014. Pts who had at least one malignancy prior to diagnosis were considered to have had secondary MM. Pts who were not receiving any treatment within first 6 months after the diagnosis and still alive were considered to have had SM. Overall survival (OS) was estimated by the Kaplan-Meier method and compared with the log-rank test. Cumulative incidence of progression from SM to symptomatic MM was calculated with death as competing risk and compared with the Gray's test. Multivariale Cox and logistic regression analyses was used to identify independent predictors of OS and progression from SM to symptomatic MM, respectively.
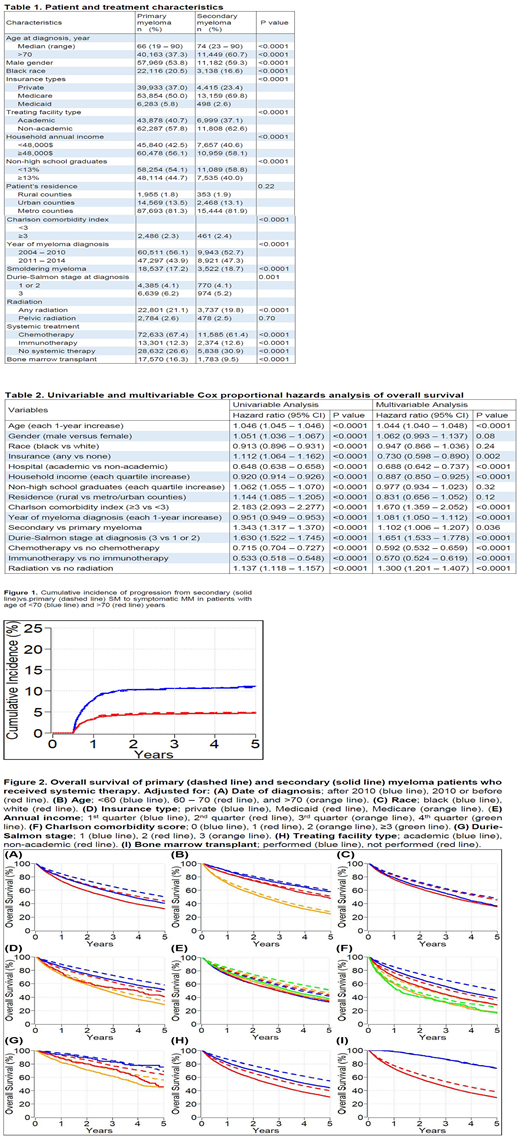
Results: We identified 126,672 MM pts, 22,064 (17%) were SM, 18,864 (15%) were secondary MM, 57,529 (45%) were female, 26,256 (20%) were black, and 56,225 (44%) were diagnosed after 2010. Median age at diagnosis was 67 years (range: 19 - 90). The Charlson comorbidity index was 0, 1, and ≥2 for 96,554 (76%), 20,287 (16%), and 9845 (8%) pts, respectively. Durie-Salmon stage at diagnosis was unavailable, 1, 2, and 3 for 113,917 (90%), 2148 (2%), 3007 (2%), and 7613 (6%) pts, respectively. Patient and treatment characteristics are compared between primary and secondary MM in Table 1. Median age and percentages of pts with age >70 were higher in secondary MM (74 vs 66 and 61% vs 37%, p <0.0001 for both). More pts with primary MM received chemotherapy (67% vs 61%, p <0.0001) and bone marrow transplant (16% vs 10%, p <0.0001) compared to secondary MM.
Median follow-up time of alive pts was 46 months. Five-year cumulative incidence of progression from secondary vs primary SM to symptomatic MM in pts with age of ≤70 and >70 years were 11.1% (95% CI: 9.3 - 12.9) vs 10.8% (95% CI: 10.2 - 11.4), p=0.89, and 4.7% (95% CI: 3.8 - 6.0) vs 4.9% (95% CI: 4.4 - 5.4), p=0.52, respectively (Figure 1). On multivariable analysis, only each 1-year decrease in age (OR 1.002, 95% CI: 1.002 - 1.003, p<0.001) was independently associated with progression of SM to symptomatic MM, after adjustment for secondary vs primary SM (OR 1.001, 95% CI: 0.992 - 1.011, p=0.77) and male vs female gender (OR 1.005, 95% CI: 0.998 - 1.012, p=0.17).
Five-year OS of pts with primary and secondary MM who received systemic therapy were 46.2% (95% CI: 45.8 - 46.6) and 35.7% (95% CI: 34.7 - 36.7), respectively (p <0.0001). Figure 2 shows the comparison of OS between primary and secondary MM who received systemic therapy in several subgroups. Five-year OS of secondary vs primary MM pts in transplant and no-transplant cohorts were 73% (95% CI: 71 - 76) vs 73% (95% CI: 72 - 74), p=0.30, and 29% (95% CI: 28 - 30) vs 38% (95% CI: 37 - 38), p<0.0001, respectively (Figure 2-I). On multivariable analysis, each 1-year increase in age, any vs no insurance, academic vs non-academic hospital, each 1-quartile increase in household income, Charlson comorbidity index ≥3 vs <3, each 1-year increase in year of MM diagnosis, secondary vs primary MM, SM vs symptomatic MM, Durie-Salmon stage 3 vs 1/2, treatment with radio-, chemo- and immunotherapy were independent predictors of OS (Table 2).
Conclusion: Here, we showed that the risk of progression of SM to symptomatic MM is not dependent on previous cancer therapy suggesting a potential lack of cause-and-effect association between chemotherapy/radiation and initial myelomagenesis. Also, secondary MM has worse prognosis than primary MM after adjusting for known unfavorable prognostic factors highlighting potential host-related factors predisposing to poor outcomes. Importantly, previous cancer was not an adverse prognostic factor for more fit and transplant-eligible pts who received bone marrow transplant.
Malek:Janssen: Speakers Bureau; Amgen: Speakers Bureau; Adaptive: Consultancy; Medpacto: Research Funding; Sanofi: Consultancy; Takeda: Consultancy; Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal