Introduction:
MYC rearrangements (MYCr) occur in 5 to 15% of diffuse large B-cell lymphomas (DLBCL) and 20 to 35% of high-grade B-cell lymphoma, NOS (HGBL-NOS), are a defining criterion of the category HGBL with rearrangements of MYC and/or BCL2/BCL6 (HGBL, with MYCr and BCL2/BCL6), and may be present in 90% of Burkitt lymphoma. The current WHO classification considers cytogenetic techniques as the appropriate tool to detect MYCr but does not define how to approach to the identification of such alteration. As the global incidence of MYCr in large B-cell lymphomas (LBCL) is low, it is necessary to clarity whether FISH or other cytogenetic methods have to be applied to all LBCL or only in selected cases. We previously identified LMO2 as a potential surrogate marker of MYCr in LBCL (Colomo L, Am J Surg Pathol 2017). Our aim with this study is to confirm this observation and evaluate the clinical impact of this marker in the survival of patients with LBCL.
Methods:
We have prospectively studied between September 2014 and July 2019 a new series of 180 LBCL including patients with DLBCL, HGBL, with HGBL, with MYCr and BCL2/BCL6, HGBL-NOS and transformed low-grade lymphomas into DLBCL (tDLBCL) diagnosed according to WHO criteria. LMO2 (clone 1A9-1), MYC (clone Y69) and a common immunohistochemistry (IHC) panel of B and T-cell markers have been used for the histological categorization of the cases, using whole tissue sections. The cutoff for LMO2 and MYC were 30% and 40%, respectively. MYC and BCL6 genes were studied using break apart probes, and BCL2 gene using dual-color dual-fusion probes (IGH/BCL2), all from Vysis-Abbott. We have statistically correlated the loss of expression of LMO2 and the overexpression of MYC with the presence or absence of MYCr. Moreover, we performed survival analyses assessing the clinical impact of LMO2 in a series of 162 LBCL patients (112 DLBCL, 20 HGBL, with MYCr and BCL2/BCL6, 4 HGBL-NOS and 26 tDLBCL). The survival series included cases diagnosed before 2014 with IHC and FISH data.
Results:
The prospective series included 132 patients with DLBCL (78M/52F; median age 67 years, range 35-95), 9 HGBL, with MYCr and BCL2/BCL6 (5M/4F; median age 67 years, range 42-85), 4 HGBL-NOS (2M/2F; median age 58 years, range 42-89), and 35 tDLBCL (31 transformed follicular lymphomas, 3 marginal zone lymphoma and 1 lymphoplasmacytic lymphoma; 23M/20F; median age 64 years, range 40-82).
LMO2 and MYC were expressed as follows, respectively: 84/130 (65%) and 46/132 (35%) in DLBCL; 1/9 (11%) and 8/9 (89%) in HGBL, with MYCr and BCL2/BCL6; 0/4 and 3/4 (75%) HGBL-NOS; 25/34 (73%) and 7/33 (21%) tDLBCL. MYCr were identified in 9/132 (7%) DLBCL; all HGBL, with MYCr and BCL2/BCL6; 4/4 HGBL-NOS; 7/35 (20%) tDLBCL.
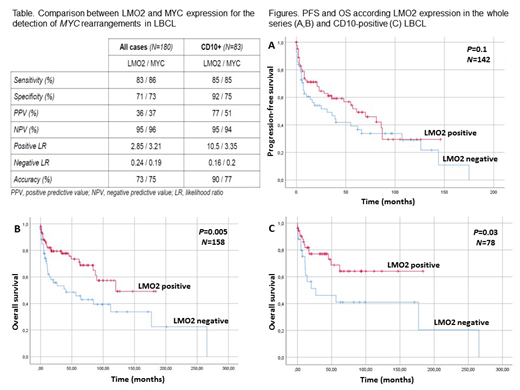
The table shows the comparisons between LMO2 and MYC protein expression for the identification of the presence of MYCr in the series of LBCL. Whereas in the whole series LMO2 and MYC had similar results, among CD10-positive cases, LMO2 had better results than MYC and identified better the presence of MYCr than MYC protein expression.
The 5-year progression-free survival (PFS) according the diagnostic categories was 59% for DLBCL, 28% for HGBL, with MYCr and BCL2/BCL6, 25% for HGBL-NOS and 22% for tDLBCL (P=0.015). In addition, PFS was significantly lower for the presence of MYCr (26% vs 53%, P=0.02) and MYC IHC expression (35% vs 53%, P=0.005), and showed a positive trend for LMO2 loss of expression (39% vs 52%, P=0.1). The 5-year overall survival (OS) according the diagnostic categories was 67% for DLBCL, 23% for HGBL, with MYCr and BCL2/BCL6, 50% for HGBL-NOS and 77% for tDLBCL (P<0.001). In addition, OS was significantly shorter for the presence of MYCr (37% vs 71%, P=0.002), MYC protein expression (46% vs 75%, P=0.001), and for LMO2 loss of expression (46% vs 74%, P=0.005). In a Cox regression survival analysis including IPI and LMO2 for the 68 CD10-positive cases, IPI (HR: 1.61 P=0.03) was the most important variable for predicting OS, and LMO2 showed a significant trend (HR: 0.44 P=0.06). However, the addition of MYC IHC and MYCr did not add predictive accuracy to IPI score (HR: 1.6 P=0.31; HR: 1.8 P=0.19, respectively).
Conclusions:
LMO2 detection by IHC is a useful tool to detect MYCr in aggressive LBCL, particularly in CD10-positive cases. Moreover, LMO2 protein expression captures the prognostic significance of the different diagnostic histological categories and the presence of MYCr in this group of lymphomas.
Sanchez-Gonzalez:Alexion: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Shire: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Salar:Celgene: Consultancy; Gilead: Consultancy, Speakers Bureau; Janssen: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal