Background: Peripheral T cell lymphoma (PTCL) and Extranodal NK/T cell lymphoma (ENKTCL) are rare types of non-Hodgkin's lymphoma (NHL), with a higher incidence in Asian countries. Outcomes for patients (pts) with relapsed or refractory(R/R) PTCL and ENKTCL are very poor, there is still lack of effective treatment for this patients population. Mitoxantrone is a syntheticc anthracenedione anticancer drug, which is effective on lymphoma, leukemia and other solid tumors. Tissue distribution or accumulation in tumor tissue of hydrochloride liposome (PLM60) was increased in our preclinical investigation. The pharmacokinetic parameters especially half-life of PLM60 was prolonged significantly in phase 1 trial. Phase Ib clinical studies showed good results of PLM60 in relapsed NHL. Therefore, we conduct this phase II clinical studies to evaluate the efficacy and safety of PLM60 in patients with R/R PTCL and ENKTCL. At present time, this is the first clinical study to evaluate PLM60 in treating R/R PTCL and ENKTCL worldwide.
Methods: This is a single-arm, open-label, multi-center, phase II clinical study. The major inclusion criteria include age≥18 years old, pts with histologically confirmed PTCL (mainly including peripheral T cell lymphoma, NOS,PTCL-U; angioimmunoblastic T-cell lymphoma,AITL; anaplastic large cell lymphoma,ALCL; and other invasive NHL derived from T cells) and ENKTCL that was treated at least 1st line of chemotherapy, ECOG performance status 0 or 1. The main exclusion criteria included cumulative dose of doxorubicin >360mg/m2 and patients has clinically significant cardiac malfunction and uncontrollable underlying cardiovascular diseases. PLM60 20mg/m2 was administered intravenously , every 4 weeks for up to 6 cycles or until disease progression, intolerable toxicity, death or withdrawal due to the investigator's decision. The primary endpoint was objective response rate (ORR) based on investigator and independent central review (ICR) per Criteria for Response Assessment of Hodgkin and non-Hodgkin Lymphoma 2007. Secondary endpoints included duration of response (DoR), progression-free survival (PFS), overall survival (OS), disease control rate (DCR) and safety. Adverse events will be rated according to the NCI Common Terminology Criteria for Adverse Events (CTCAE) 4.03. This trial is registered at ClinicalTrials.gov, number NCT03776279.
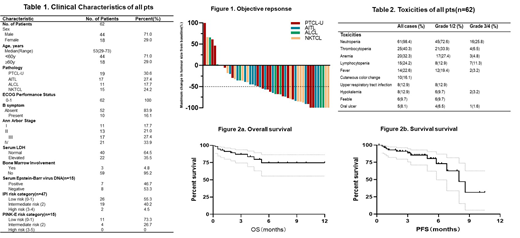
Results: 62 eligible patients were treated in 18 institutions in China between April 2018 and July 2019. Patient characteristics are summarized in Table 1. Median number of previous chemotherapy regimens was 2(1-7). At the cut-off day of July 20, 2019, 9 pts remained on treatment and 3 pts withdrew due to protocol violation and lost follow-up. 50 patients were evaluable for response, the investigator-assessed ORR was 54.0%(27/50)with CR rate 20.0%(10/50) (CR). The subtype CR rate were 17.6%(3/17), 17.6%(3/17), 18.2%(2/11), 13.3%(2/15)for PTCL-U, AITL, ALCL and ENKTCL respectively. The ORR were 42.1%(8/17), 42.1%(8/17), 45.5(5/11), 40.0(6/15), respectively (Figure 1). The median time to response was 8 weeks (ranged from 4 to 24 weeks) . Median follow-up was 3.8 (ranged from 0.2 to 14.4 m) months. Median PFS was 8.0months (95% CI, 6.1-9.9m), with a 6-month PFS rate of 73.1±9.4%. Median OS was not reached, with a 6-month OS rate of 77.3±6.9%(Figure 2a,b). All-grade treatment-emergent adverse events (TEAEs) are listed in Table 2. The most common toxicity of PLM60 was myelosuppression. The most common grade 3/4 toxicity(>10% TEAEs) was neutropenia(25.8%) and lymphocytopenia(11.3%). There were no treatment-related deaths.
Conclusion:PLM60 monotherapy yielded promising results for patients with R/R PTCL and ENKTCL with moderate toxicities. Further investigation is urgently needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal