Introduction: Several patient and disease biology characteristics that impact overall survival (OS) outcomes of patients with newly diagnosed multiple myeloma (NDMM) have been well described. However, several prior population-based registry studies in the US such as SEER and NCDB databases have demonstrated the negative prognostic impact of socio-economic (SE) factors such as low median household income based on US national census bureau data for zip code of residence as well as absence of marital support on the OS of NDMM patients. Whether such SE factors are independent of established host and disease biology related factors remains unknown due to the absence of detailed patient-level data in population-based cancer registries. Thus, we evaluated whether such SE factors independently affected the OS of NDMM patients in our institution when accounting for patient and disease biology related factors.
Methods: We analyzed a retrospective cohort of consecutive NDMM patients seen at the Mayo Clinic from January 2005 to December 2015. Median household income for each patient's area of residence was estimated by matching their home zip code at diagnosis with data available through the US National Census Bureau. Median household income < $63,000 for a zip code were used to classify patients as having low income based on the National Cancer Database classification of the bottom three quartiles. Absence of marital support was considered in patients divorced, single or widowed at the time of diagnosis. Survival estimates were calculated using the Kaplan-Meier method. Patient and disease biology related factors taken into consideration included age, FISH cytogenetics, ISS stage and LDH levels. Survival estimates were compared between groups using the log-rank test. Multivariable adjusted proportional hazards regression models were fit for the association between known prognostic factors and OS.
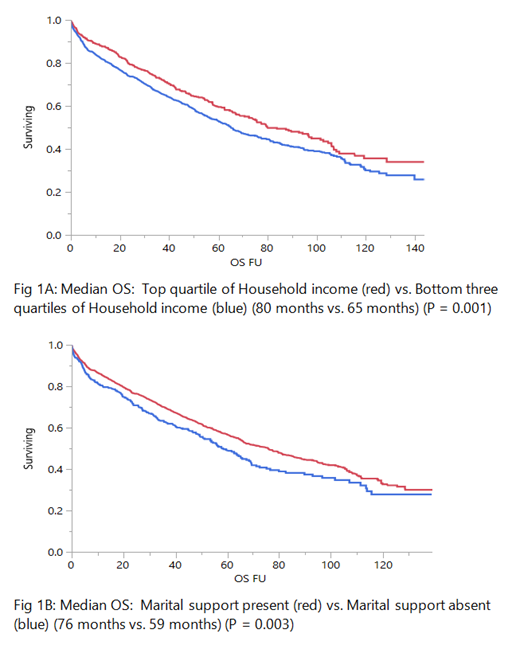
Results: A total of 2,621 MM patients were analyzed from the Mayo Clinic cohort of which 60% were male and the median age was 64 (22 - 96) years with 14% being 75 years of age or older. In this cohort, 541 (33%) patients had ISS 3 disease and 370 (22%) had high risk cytogenetics by FISH. The median OS based on estimated average household income was 65 months for the group of patients with low household income (N = 32%) and 80 months for the remainder (P = 0.001) (Fig 1A). The median OS based on marital support was 59 months for those without marital support at diagnosis (N = 21%) versus 76 months for remainder (P = 0.003) (Fig 1B). However, in a multivariable analysis that included the aforementioned SE factors and patient and disease biology characteristics , only age of 75 years or older (p < 0.001), the presence of high-risk FISH cytogenetics (p < 0.001), presence of ISS 3 disease (p < 0.001) and elevated LDH (p = 0.005) retained independent statistical significance in predicting for worse OS. Lower household income (p = 0.264) and absence of marital support (p = 0.054) were not independent predictors of worse OS.
Conclusions: With the caveat of patient selection bias in a tertiary academic center, SE factors such as estimated average household income and marital support at diagnosis do not appear to impact OS of NDMM patients when considered in the context of traditional host and disease biology risk factors. These findings are in contrast to those suggested by population based registry studies; nevertheless, similar patient-level assessments should be considered in patient cohorts from non-tertiary medical centers as these results may likely be different.
Dispenzieri:Akcea: Consultancy; Intellia: Consultancy; Janssen: Consultancy; Pfizer: Research Funding; Takeda: Research Funding; Celgene: Research Funding; Alnylam: Research Funding. Dingli:alexion: Consultancy; Janssen: Consultancy; Millenium: Consultancy; Rigel: Consultancy; Karyopharm: Research Funding. Lacy:Celgene: Research Funding. Kapoor:Amgen: Research Funding; Glaxo Smith Kline: Research Funding; Sanofi: Consultancy, Research Funding; Celgene: Honoraria; Janssen: Research Funding; Cellectar: Consultancy; Takeda: Honoraria, Research Funding. Leung:Prothena: Membership on an entity's Board of Directors or advisory committees; Aduro: Membership on an entity's Board of Directors or advisory committees; Takeda: Research Funding; Omeros: Research Funding. Russell:Imanis: Equity Ownership. Gertz:Medscape: Consultancy, Speakers Bureau; Research to Practice: Consultancy; Springer Publishing: Patents & Royalties; Ionis/Akcea: Consultancy; Pharmacyclics: Membership on an entity's Board of Directors or advisory committees; Alnylam: Consultancy; Prothena Biosciences Inc: Consultancy; Celgene: Consultancy; Janssen: Consultancy; Spectrum: Consultancy, Research Funding; Annexon: Consultancy; Appellis: Consultancy; Amgen: Consultancy; Physicians Education Resource: Consultancy; Abbvie: Other: personal fees for Data Safety Monitoring board; Teva: Speakers Bureau; Johnson and Johnson: Speakers Bureau; DAVA oncology: Speakers Bureau; Proclara: Membership on an entity's Board of Directors or advisory committees; i3Health: Other: Development of educational programs and materials; Amyloidosis Foundation: Research Funding; International Waldenstrom Foundation: Research Funding. Kumar:Celgene: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal