Introduction: Patients with high-risk multiple myeloma (HRMM) who have undergone autologous stem cell transplant (ASCT) will inevitably relapse and have a progression free survival (PFS) ranging from 8-14 months (Gaballa et al, American Journal of Hematology, 2016) and 24-39 months while on lenalidomide (Len) maintenance therapy (Jackson et al, The Lancet Oncology, 2019). Unlike in solid tumors, PD-1 blockade has no single agent activity in relapsed and refractory multiple myeloma (MM) patients suggesting that immune stimulating agents, immunomodulatory agents (IMiDs), such as lenalidomide (Len) or pomalidomide (Pom) are necessary in combination with anti-PD-1 blockade to increase depth and duration of response post-ASCT. The Keynote-023 study revealed an overall response rate (ORR) of 76% with the combination of pembrolizumab (Pem), Len and dexamethasone (Dex). Similarly, the Keynote 135 study using the combination of Pem, Pom, and Dex revealed an ORR of 60%. Unfortunately, the phase III studies comparing an IMiD vs Pem with the IMiD upfront at the early relapsed setting were halted because of increased deaths on the Pem arm and a decreased median PFS. With our Phase II study currently on clinical hold by the FDA, we are presenting here the 2-year follow-up of the original patient cohort including some preliminary safety and efficacy data of Pem-Len-Dex in HRMM patients as post-ASCT consolidation (NCT02906332).
Methods: Patients with HRMM who have undergone induction therapy followed by single or tandem melphalan-based ASCT were considered eligible 2-6 months post ASCT. HRMM criteria are defined by any of the following: ISS stage 3; del 13q by cytogenetics; FISH with 1q amplification, 1p deletion (del), p53 del, t(4;14), t(14;16), t(14;20), hypodiploidy; or a high-risk gene expression profile score. Patients were excluded if they had progression of disease at time of screening or if there was evidence of organ dysfunction. Patients received Pem 200 mg IV at day 1;Len 25 mg po daily at days 1-14; and Dex 40 mg daily at days 1,8,15 of a 21-day cycle for a total of 2 cycles and then an additional 2 cycles of Pem + Len without Dex at the same dose and frequency. Survival outcomes post-ASCT were measured using the log-rank test.
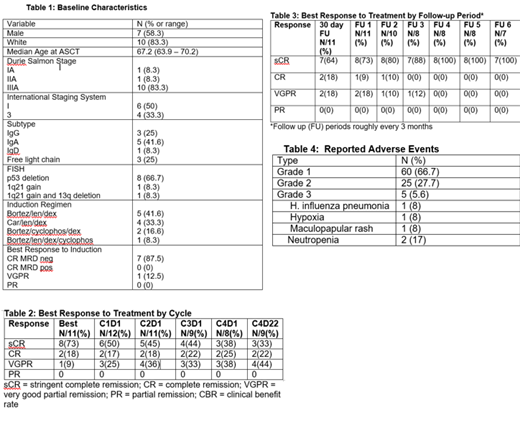
Results: Of 15 patients screened, 12 received at least one dose of therapy and were deemed evaluable. One patient withdrew consent and did not follow up after cycle 2. Baseline characteristics are shown in Table 1. Thirty-three percent were ISS 3, 66.7% had a p53 deletion by FISH, 41.6% received induction Bortezomib-Len-Dex; 33% received induction Carfilzomib-Len-Dex, and the remaining 24.9% received other bortezomib-based induction. Best ORR during the 2 year follow up showed 8 patients (73%) achieving stringent complete remission, 2 patients (18%) showing complete remission and 1 (9%) achieving very good partial remission. Table 2 shows best response to treatment by cycle of therapy. Table 3 shows best response during follow-up visits, which were 3 months apart. Of the 11 patients who completed therapy, 8 had minimal residual disease (MRD) status assessed and among them, 7 were MRD negative by flow cytometry, tested 30 days after the fourth cycle. With a median follow-up of 32.2 months, median PFS was 27.6 months. The PFS rates at 1 year and 2 year are 91.3% and 65.2%, respectively. All patients had adverse events (AEs), AEs were attributed to Pem, Len, or Dex rather than from ASCT. Of the 90 AEs that were reported, 5.6% were grade 3 and 94% were grade 1 or 2 (Table 3). The most common hematologic AE was neutropenia (41.7%), with 3 pts (25%) grade 1 and 2, and 2 pts (16.6%) grade 3. The most common non-hematologic AEs were intermittent constipation (16.6%), diarrhea (16.6%), fatigue (8.3%), and increased ALT (8.3%) and were graded as 1 or 2. Non-hematologic grade 3 AEs occurred in 2 pts and included hypoxia and maculopapular rash. There was 1 serious AE, H. influenza pneumonia requiring inpatient admission, which was not considered to be related to Pem.
Conclusions: The combination of Pem, Len, and Dex given to HRMM patients in the post-ASCT consolidation setting is well tolerated. In comparison to historical controls of HRMM patients post-ASCT with a median PFS of 8-14 months, the PFS rates of 91.3% and 65.2% at 1 and 2 year post-ASCT respectively suggest an efficacy signal for the use of Pem, Len, and Dex as post-ASCT consolidation. Larger prospective studies are needed to validate these results.
Siegel:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Bristol-Myers Squibb Company: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Rowley:Allergan: Equity Ownership; Fate Therapeutics: Consultancy. Biran:Amgen: Consultancy, Honoraria, Research Funding; Merck: Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Bristol Meyers Squibb: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal