Introduction: Juvenile myelomonocytic leukaemia (JMML) is a clonal haematopoietic disorder occurring in pediatric age group usually characterized by uncontrolled granulocytic and monocytic lineage proliferation and a poor outcome. JMML is characterised by aberrant signal transduction of the RAS signalling pathways, usually manifesting in molecular alteration of one of the five cardinal genes: NF1, NRAS, KRAS, PTPN11 and CBL. Recent high-throughput studies have started to push the horizon of JMML associated mutations wider and have proposed molecular-based risk algorithms. We comprehensively evaluated the genomic profile of JMML that were referred to our hospital for diagnosis and treatment.
Methods: We developed a 51 gene (103 kB) low-cost targeted sequencing myeloid panel based on single molecule molecular inversion probes. This focussed panel interrogated sets of genes implicated in pathogenesis of myeloid malignancies. A total of 50 children with clinical and pathological features of JMML were sequenced at high coverage using this assay on an Illumina MiSeq.
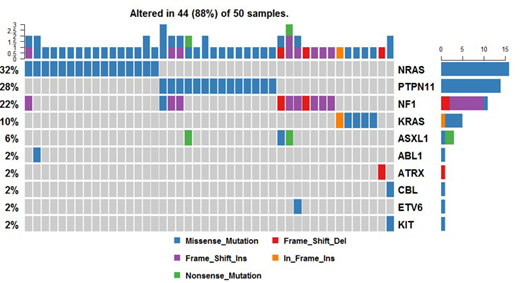
Results:The median age of our cohort was 2 years, with a male preponderance. Among the 50 patients, 43 (86%) harboured mutations in one of the RAS/MAPK pathway genes. The most frequently mutated gene in our cohort was PTPN11 (14, 28%), and NRAS (14, 28%), followed by NF1 mutation in 22% (11) cases (Figure 1). Interestingly, 20% (10) of children had more than one mutation, with 5 cases harbouring two RAS pathway mutations. Of these 5 patients, one patient harboured two coexistent mutations in the NF1 gene, three patients had coexistent PTPN11 and NF1 mutations and one patient had a coexistent NF1 and NRAS mutations. Additionally, two patients also had an ASXL1 mutation, coexistent with NF1 and NRAS mutations respectively. Other non-RAS pathway mutations involved ABL1, ATRX, SETBP1, SH2B3 and ZRSR2 genes. The median variant allele frequency of RAS pathway mutations detected was 40.75%. Monosomy 7 was detected in 32% (16) patients, and five of these did not harbour any RAS pathway mutations. The follow up data revealed that 37 (74%) of these patients have succumbed to the disease. In our cohort, only five patients received an allogenic stem cell transplant, owing to economic constraints; two of these patients have succumbed to the disease. The median time period from diagnosis to death was 7.2 months in the cohort. On survival analysis, patients with PTPN11 mutations showed a trend to shorter overall survival, compared to their wildtype counterparts (p=0.7, median OS 10.6 months vs 38.1 months). Additionally, patients harbouring more than one mutation also showed a trend to shorter OS (p=0.64, median OS 10.3 months vs 38.1 months). Among the thirteen patients who are still on regular follow-up, two patients have relapsed with disease progression to acute myeloid leukemia and T/myeloid mixed phenotypic acute leukemia respectively.
Conclusion: Our study represents the largest cohort of JMML from a single centre in the Indian subcontinent. This study depicted that almost 90% cases of JMML harbor at least one mutation with 86% harbouring at least one RAS pathway mutation. Presence of PTPN11 mutations and co-existence of more than one mutation may be the major determinants of outcome in JMML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal