Introduction:Cardiovascular disease (CVD) is an important cause of morbimortality in patients with low risk myelodysplastic syndrome (LR-MDS). Up to 70% of patients suffer cardiovascular events and heart disease is the second cause of death in this context. Cardiac damage etiology is complex and multifactorial in this group of patients. Iron overload cardiomyopathy (IOC) due to transfusion dependency is the most well identified factor in this setting, however other circumstances such as vascular aging, cardiac reserve reduction and high cardiac output related to chronic anemia, among others, play an important role in this population. Thus, despite its importance in MDS patients, prognostic cardiovascular predictive factors are not adequately identified, and cardiac monitoring in these patients is not sufficiently stablished. Therefore, our objectives were to determinate the prevalence and characterization of CVD in LR-MDS patients, to analyze their mortality and cardiovascular prognosis and to identify predictors of cardiovascular events or death (combined event, CE) in this setting.
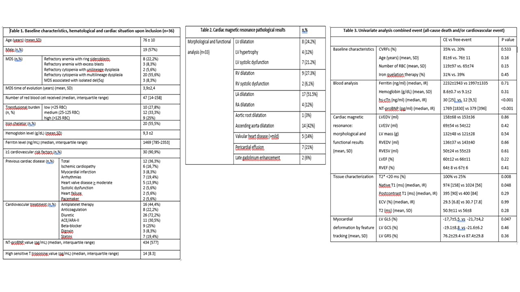
Material and methods: A prospective single center study with 36 LR-MDS patients (31 of them in transfusion requirements) was conducted. All patients underwent a complete hematological and cardiological assessment including ECG, cardiac biomarkers (N-terminal pro b-type natriuretic peptide (NT-proBNP) and high-sensitive cardiac T troponine (hs-cTn)) and cardiac magnetic resonance (CMR) with parametric sequences (T1, T2 and T2* mapping) and myocardial deformation by feature tracking (FT). Univariate and multivariate analysis including clinical, analytical and imaging factors for predicting the combined cardiovascular event (heart failure (HF), arrhythmia or ischemic heart disease) and/or all-cause of mortality (CE) was performed by Cox regression.
Results:Thirty-six patients with LR-MDS were recruited from 2016 to 2017, with a mean age of 76 ± 10 years, 53% males. Thirty-one patients (84%) were in transfusion dependency (TD). Regarding baseline characteristics for cardiovascular disease most of them (90.9%) had CV risk factors (CVRFs) and 36% suffered of previous heart disease (Baseline characteristics, hematological and cardiac situation at inclusion in table 1). Cardiac assessment revealed high prevalence of structural heart disease, in most of cases previously unknown and significant incidence of CV events during the follow-up. Thus, Cardiac MR detected high prevalence structural heart disease (table 2). As a result of this first cardiac assessment, 15 patients (42%) required modifications in their cardiovascular treatment and most of cases needed to start cardiovascular treatment. After a median follow up of 2.2 years, 35.5% of TD patients suffered the CE, 16% died and 32% presented cardiovascular events: HF 13.9%, pacemaker implantation due to atrioventricular block 2.8%, ischemic heart disease 5.6%, and atrial fibrillation 5.6%. In the univariate analysis for the CE (table 3), higher hs-cTn (p=0,007), higher NT-proBNP (p = 0.001), T2* <20 ms (p = 0.008), lower T1 native time (p = 0.048) and higher longitudinal strain (p=0,047) were all significant negative prognostic factors for developing CE. NT-proBNP value higher than 485pg/ml (HR 96,7; IC 95% 1,135-8243; p = 0,044), native T1 time lower than 983 ms (HR 44,8; IC 95% 1,235-1623; p = 0,038) and higher LS (p=0,043) retained its independent adverse prognostic factor in the multivariate analysis for CE.
Conclusion: LR- MDS patients presented high prevalence of cardiovascular risk factors and structural heart disease and most of cases were only identified after an appropriate cardiological assessment. The presence of a CV event and/or death is very frequent during patients follow up. Cardiac biomarkers and CMR could improve the identification of patients at risk for CVD in which a cardiological treatment and follow-up could improve survival.
Díez-Campelo:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene Corporation: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal