Background
Patients diagnosed with myeloproliferative neoplasms (MPNs) are at an increased risk of vascular events. A paucity of population-based studies investigating risk factors exist. We conducted a nested case-control study to explore the relative importance of risk factors, treatment, and blood counts for vascular complications in Essential Thrombocythemia (ET) and Polycythemia Vera (PV), and their impact on life expectancy.
Patients and Methods
All newly diagnosed MPN patients (pts) are reported to the Swedish national MPN registry as mandated by Swedish law. 922 ET pts and 763 PV pts diagnosed from January 2010 through September 2015 with a 3 or 6-year follow-up were included. Pts identified as having a vascular complication were assigned a control patient matched by MPN subtype, gender and age. Blood counts, EPO and JAK2V617F mutation status at diagnosis were recorded, as was co-morbidity, smoking habits and vascular complications prior to diagnosis. At the time of vascular complication cytoreduction, anti-thrombotic therapy and blood counts were investigated. In controls these parameters were registered at the corresponding time from diagnosis. MPN therapy is recommended in Nordic guidelines that closely mirror those issued by the ELN.
Statistical analyses
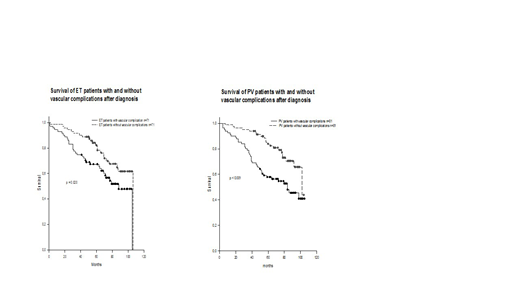
Differences in the distribution of variables were analyzed using Mann-Whitney test. Chi square test was used for comparison between groups. Overall survival estimations were calculated by Kaplan-Meier analysis and compared using Log Rank test. Multivariate analysis was performed by unconditional logistic regression.
Results
At diagnosis ET and PV pts with complications were older compared to the whole ET and PV cohorts, mean ages 73 and 65 years respectively in ET (p<0.001), 73 and 68 years in PV (p<0.001). No significant differences in blood counts, EPO, JAK2 V617F mutation status or vascular events prior to diagnosis were seen compared to the whole cohorts. Neither did cardiovascular risk factors nor smoking habits differ. The vast majority of pts in the study were high risk according to ELN criteria.
Seventy-one ET pts (8%) suffered at least one vascular complication during follow-up. 49 thromboembolic and 22 hemorrhagic; 1.4 and 0.6 events/100 patient-years respectively. Median time from diagnosis to vascular complication was 24 months (0-71). Most common thromboembolic events were cardiac, DVT/LE and cerebral. Gastrointestinal (GI) and cerebral were the most frequent hemorrhagic complications. At time of event there were no significant differences in mean hemoglobin (Hgb), hematocrit (Hct) or platelet counts. Mean white blood cell (WBC) count was 9.1 x109/L in the complication group compared to 7.1 x109/L in controls (p=0.063). Frequent use of cytoreductive therapy and/or anti-thrombotics may have contributed to a lack of difference between treated and untreated pts in ET.
81 (11%) of the PV pts had at least one vascular event after a median time of 24 months (0-89). 59 of these thromboembolic and 22 hemorrhagic; 2.5 and 0.9 events/100 patient-years respectively. Cerebral ischemic events were the most frequent, followed by DVT/LE and cardiac, in hemorrhage G-I and cerebral. At time of vascular event the mean WBC was 13.5 x109/L compared to 9.6 x109/L in controls (p<0.001). No significant differences were found in Hgb, Hct or platelets. Cytoreductive therapy was given to 51% of complication pts compared to 79% of controls (p<0.001). Similar differences were found in use of anti-thrombotic prophylaxis; 86% compared with 99% (p=0.007). In multivariate analysis, only cytoreductive therapy, odds ratio (OR) 0.26 (p=0.001) and antithrombotic therapy OR 0.10 (p=0.043) remained as significant protective factors.
The estimated 5-year survival was significantly impaired in ET pts who suffered a vascular event compared the matched controls without vascular complication, 65% and 81%, respectively (p=0.020). The same was seen in PV, 60% compared to 85% in the controls (p<0.001). Causes of death will be reported.
Conclusions
In this population-based study the main finding was that survival of PV and ET pts with vascular complications is highly reduced compared to controls. At the time of complication blood values, with the exception of WBC in PV, do not show any significance. This finding clearly demonstrates that the cytoreductive treatment per se is protective, and underscores the negative impact of undertreatment in PV.
Samuelsson:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; CTI Bio: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; AOP Pharma: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal