Introduction. Prefibrotic myelofibrosis (pre-PMF) is a unique entity in the 2016 WHO classification of myeloproliferative neoplasms with distinct clinical phenotype and outcome [Guglielmelli P, Blood 2017]. Compared to essential thrombocythemia (ET), pre-PMF is characterized by more pronounced disease manifestations, adverse mutation profile and worse outcome. Previous studies [Rumi E, Oncotarget 2017] showed that patients (pts) with pre-PMF present a risk of vascular events similar to ET. However, no studies performed a comprehensive assessment of risk factors for thrombosis in pre-PMF. The current study aimed to identify risk factors for thrombosis and bleeding in a large series of pre-PMF pts and explore the effectiveness of contemporary prognostic models developed specifically for ET.
Patients and Methods. The study included 382 pre-PMF pts, diagnosed by 2016 WHO criteria, referred by 4 Italian Centers. Previously published methods were used to genotype JAK2, MPL, CALR, EZH2, ASXL1, IDH1/2 and SRSF2; a high molecular risk (HMR) category was defined according to Vannucchi A, [Leukemia 2013]. Thrombosis‐free survival (TFS) was determined from diagnosis to the first thrombotic event. Pts were grouped according to the conventional risk stratification system [Barbui T, JCO 2011], IPSET‐thrombosis [Barbui T, Blood 2012] and revised IPSET‐thrombosis [Barbui T, BCJ 2015]. Cox-regression model was used for univariate analysis. Harrell's concordance (C) statistic was calculated to measure the incremental accuracy of multivariable models sequentially adjusted for new predictors of thrombotic risk. A P <0.05 was considered statistically significant.
Results. At diagnosis, 65 pts (17%) experienced major thrombotic events which included 35 (9%) arterial and 31 (8%) venous thromboses. With a median follow-up of 6.9 y (range 0.08-32.6), 56 (15%) pts developed an arterial or venous thrombotic event, with a total incidence rate of 1.99% pts/year (pt-y); 30 (8%) were arterial and 28 (7%) venous events with incidence rate of 1.00% pt-y and 0.95% pt-y, respectively. Splanchnic vein thrombosis (SVT) represented the most frequent venous events before/at diagnosis (26%). During the follow-up, 16% and 8% of pts experienced myelofibrotic or leukemic progression, and 105 (27%) died, with incidence rate of 2.05% pt-y, 0.95% pt-y and 3.41% pt-y, respectively.
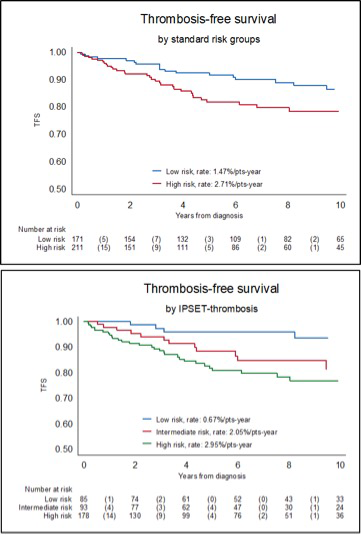
In univariate analysis, factors significant for arterial thrombosis after diagnosis were age >65y (HR 2.88; P=0.005), WBC>10x109/L (HR 2.43; P=0.026), presence of >1 generic CV risk factor (HR 2.16; P=0.047), JAK2V617F (HR 3.35; P=0.027) and HMR status (HR 13.1; P=0.027). Conversely, only history of previous thrombosis (HR 3.06; P=0.005) and previous venous event (HR 5.53; P<0.0001) retained significance for predicting venous thrombosis. Pts were effectively stratified according to IPSET and conventional risk model. The risk of thrombosis in IPSET low-, intermediate-, and high-risk categories was 0.67%, 2.05% and 2.95% pt-y, and 1.47% pt-y and 2.71% pt-y in 2-tiered thrombotic risk model. (Figure 1); in revised-IPSET, 0.54%, 2.23%, 2.44% and 2.69 %pt-y in the very low, low, intermediate- and high-risk category. When WBC>10x109/L or HMR variables were incorporated into IPSET model, the C-statistic increased significantly for the prediction of arterial events: from baseline value of 0.68 to 0.74 adding WBC and 0.91 HMR status.
The proportion of pts who experienced major bleeding was 3% prior/at diagnosis,and 7% during follow-up, with total incidence rate of 0.94% pt-y. In univariate analysis, predictors for major bleeding during follow-up were age >75y (HR 3.34; P=0.011), WBC>13x109/L (HR 2.33; P=0.035), presence of >1 generic CV risk factor (HR 2.41; P=0.035), particularly hypertension (HR 2.63; P=0.016) and grade-1 fibrosis (HR 2.28; P=0.05). High platelet count and treatment, including antiplatelet and anticoagulant drugs, did not reach statistical significance.
Conclusions. Overall, this study identified independent risk factors for major thrombosis and bleeding in pre-PMF. Of interest, we report that HMR status predicted for arterial thrombosis during the follow-up. Pre-PMF pts showed remarkably high rate of venous thrombosis, mostly represented by SVT. The 3-tiered IPSET prognostic model for thrombosis reliably predicted occurrence of thrombotic events in pre-PMF and should be considered as standard reference.
Rumi:novartis: Honoraria, Research Funding. Thiele:Shire: Research Funding; Incyte: Consultancy, Honoraria, Other: Remuneration, Research Funding; Sanofi: Consultancy, Honoraria, Other: Remuneration; Novartis: Consultancy, Honoraria, Other: Remuneration, Research Funding; AOP Orphan Pharmaceuticals: Consultancy, Research Funding. Vannucchi:Incyte: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Italfarmaco: Membership on an entity's Board of Directors or advisory committees; CTI BioPharma: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal