Introduction
Most children with acute myeloid leukaemia (AML) harbour fusion genes which are ideal targets for molecular minimal residual disease (MRD) monitoring. However, evidence of prognostic significance is currently lacking and consequently most current paediatric AML treatment protocols rely on flow cytometric (FCM) evaluation to allocate treatment. Molecular MRD techniques provide significantly greater sensitivity and specificity and could allow more accurate outcome prediction, and consequently more personalised therapy, which is highly relevant in a disease where treatment related mortality, morbidity and relapse remain significant.
Methods
Between June 2016 and February 2019, MyeChild01 enrolled 170 children aged 0-18y with newly diagnosed AML who were randomly assigned to induction therapy with liposomal daunorubicin or mitoxantrone with cytarabine with or without gemtuzumab ozogamicin. Consolidation treatment was determined by karyotype, mutational profile and MRD status.
Comprehensive centralised diagnostic assessment consisted of:
Karyotype and fluorescence in-situ hybridisation (FISH) using a custom panel of probes to detect paediatric AML-associated gene fusions.
PCR based screening for mutations in FLT3, NPM1 and CEPBA.
Targeted capture of known fusion loci and paired end sequencing.
RNA-seq using the Illumina TruSight fusion panel.
Where a fusion gene was identified, RT-qPCR assays were designed and optimised for each patient. NPM1 mutation was also used as an MRD target if present. Paired PB and BM samples were requested after each cycle of treatment. Patients could have sequential monitoring after completion of therapy although this was not mandated.
For this analysis, patients with core-binding factor (CBF) leukaemias i.e. inv(16)(p13q22) or t(8;21)(q22q22) with transcript levels above previously defined thresholds (Yin et al, 2012) were considered MRD positive. For all other targets, amplification in at least 2/3 replicates at <40 PCR cycles in either PB or BM was considered MRD positive.
For patients with CBF or NPM1 mutation, both molecular and FCM MRD status contributed to treatment allocation. Otherwise, FCM MRD was used unless there was no FCM target. Allogeneic stem cell transplantation (HSCT) was recommended for all patients with poor risk cytogenetics, those with intermediate risk cytogenetics who were MRD positive after cycle 2, and those with favourable risk cytogenetics who were MRD positive at the end of cycle 3. After completion of treatment, no specific advice was given regarding management of positive MRD results.
Results
We identified fusion genes in 126/170 patients (74%). We designed 55 unique RT-qPCR assays to specifically amplify 27 fusions with calculated sensitivity between 1:104 and 1:106. 62/126 children provided a complete set of samples: 31 (60%) with favourable, 18 (29%) with intermediate and 13 (21%) with high risk cytogenetic / molecular profiles.
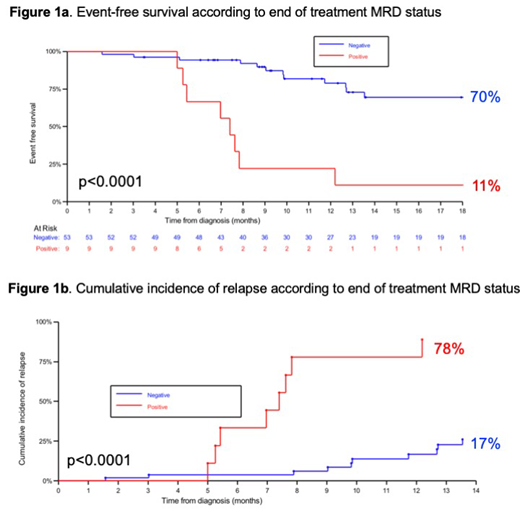
We analysed the effect of molecular MRD status at the end of protocol specified treatment, which included SCT in 17/62 (27%). One year event-free survival from diagnosis was 70% (95% confidence interval 52-82%) in patients who tested MRD negative compared to 11% (1-39%) in patients who tested MRD positive at the end of treatment (p<0.0001, figure 1a). Estimated cumulative incidence of relapse was 17% (7-30%) in patients who tested MRD negative vs 78% (28-95%) in those testing positive (p<0.0001 figure 1b). MRD status at earlier time points had less impact, possibly due to treatment intensification for MRD positivity.
Four patients received non-protocol specified SCT due to physician / family preference based on persistently positive or serially rising transcript levels after completion of treatment. At last follow up 4/4 were alive in complete remission.
Rising transcript levels were observed in a further 8 patients to whom no pre-emptive treatment was given due to individual preference or lack of appropriate therapy. Haematological relapse subsequently occurred in 8/8.
Conclusion
Molecular MRD monitoring is feasible in the majority of children with AML, permitting refinement of response-adapted therapy. Molecular MRD status at the end of treatment is highly predictive of outcome, identifying molecular complete remission as a treatment goal for these children. Serially rising MRD levels reliably predict relapse in the absence of therapeutic intervention.
Dillon:Abbvie: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; TEVA: Consultancy, Honoraria. Vyas:Astellas: Speakers Bureau; Abbvie: Speakers Bureau; Forty Seven, Inc.: Research Funding; Celgene: Research Funding, Speakers Bureau; Novartis: Research Funding, Speakers Bureau; Pfizer: Speakers Bureau; Daiichi Sankyo: Speakers Bureau. Amrolia:UCLB: Patents & Royalties. Baruchel:Bellicum: Consultancy; Servier: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Novartis: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal