The gene that encodes DNA methyltransferase 3A (DNMT3A) is mutated in nearly 40% of normal karyotype acute myeloid leukemia (AML) patients. More importantly, DNMT3A mutations are almost invariably the initiating event for the disease; however, the mechanisms by which they contribute to AML initiation are not yet clear [1, 2]. Regardless, ancestral clones containing the DNMT3A mutation are hard to eradicate, and often persist in clinical remission [3, 4]. We have recently shown that the most common DNMT3A mutation in AML patients (R882H; R878H in mice) is a dominant negative mutation that causes a focal, canonical pattern of DNA hypomethylation that is present in pre-leukemic hematopoietic cells, and appears to evolve further in fully transformed AML cells [5]. However, it is not yet clear how the DNMT3AR882H mutation can cause the clonal expansion of HSPCs, or how it makes HSPCs more susceptible to transformation by secondary mutations.
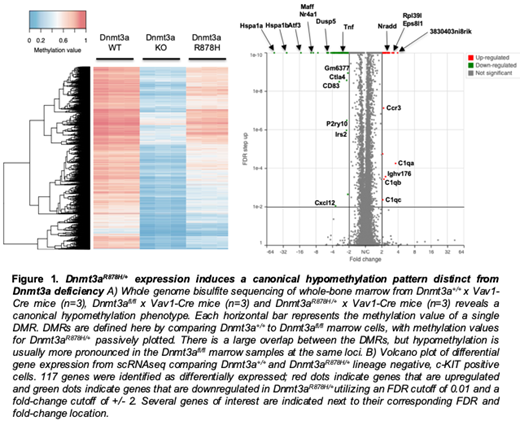
We have utilized the conditional Dnmt3aR878H knock-in model described by Guryanova et. al. [6] and established an hematopoietic-specific model of clonal hematopoiesis driven by DNMT3AR882 mutations. With this model, we set out to investigate the epigenetic and functional consequences of Dnmt3aR878H expression in murine hematopoietic cells. The bone marrow cells of 6-week-old Dnmt3aR878H x Vav1-CREmice are >95% floxed; although these mice have a distinct focal hypomethylation phenotype, it is not as striking as that of Dnmt3a deficient bone marrow cells (this is expected, since the dominant negative R882H mutation reduces DNMT3A activity by 80%, not 100%). Importantly, Dnmt3aR878H and WT RNA are expressed at a precise 50:50 ratio, mimicking the ratio found in human patients with this mutation [7]. To establish the "baseline" methylation status of Dnmt3a+/+ vs. Dnmt3aR878H/+ bone marrow cells, we harvested marrow from 6-week-old littermates and performed whole genome bisulfite sequencing on 7 independent mice from each genotype. The R878H bone marrow cells have focal, canonical regions of DNA hypomethylation that strongly resemble those seen in human patients with DNMT3AR882 mutations. 2,621 differentially methylated regions (DMRs) exist in the Dnmt3aR878H/+ marrow samples, and >99% are hypomethylated. Dnmt3a-/- bone marrow cells have > 8,000 DMRs compared to Dnmt3a+/+ bone marrow cells, highlighting the intermediate methylation phenotype in Dnmt3aR878H marrow (Figure 1A). Further, the hypomethylation phenotype is stable with aging, and does not progress between weeks 2 and 52 of life (data not shown).
Previous studies utilizing bulk RNA sequencing demonstrated very few differentially expressed genes (DEGs) in primary human AML samples with DNMT3AR882H. Therefore, we utilized single cell RNA sequencing to identify DEGs in the progenitor populations of Dnmt3aR878H hematopoietic cells. In addition to the methylation phenotype outlined above, we have identified a set of 117 DEGs (30 genes up and 87 genes down) in lineage negative, c-KIT positive cells from Dnmt3aR878H bone marrow, including Hspa1a and Hspa1b, Cxcl2 and Cxcl12, Fosb and C1q complement genes, with pathway analyses suggesting dysregulation of the proteasome, chemokine and inflammatory signaling, and apoptotic and proliferative pathways (Figure 1B). These pathways have all been implicated in cancer, and may provide a rationale for the Dnmt3aR878H -driven pre-leukemic phenotype.
Extensive hematopoietic immunophenotyping has revealed subtle population changes in progenitor and stem populations of 6-week old Dnmt3aR878H mice; we identified significantly lower granulocyte-monocyte progenitors (GMP) and multipotent progenitors (MPP), and a significant increase in SLAM cells. Although these differences are significant, they do not result in any gross lineage population skewing in the bone marrow or peripheral blood. In sum, these data define some of the epigenetic consequences of the Dnmt3aR878H mutation in hematopoietic cells, and establish this mouse model as a valid one for the study of this mutation. This is the first report of the pre-leukemic state mediated by Dnmt3aR878H and these data have important implications in the design of future pharmacological agents targeting this mutation in patients with AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal