Background: Sickle cell disease (SCD) is an inherited disorder in which pathology is driven by hemoglobin (Hb) polymerization and red blood cell sickling, leading to chronic hemolysis and anemia as well as episodic vaso-occlusion. These manifestations of SCD contribute to the cumulative organ damage that leads to disability and accelerated mortality.
Voxelotor is a first-in-class therapy in development for the treatment of SCD that has been shown to increase Hb levels and reduce markers of hemolysis, consistent with inhibition of sickle Hb polymerization. The objective of this analysis was to evaluate the association between Hb response and markers of hemolysis in voxelotor-treated patients.
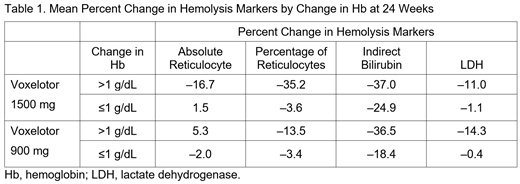
Methods: The HOPE trial is a phase 3, randomized, placebo-controlled, double-blind, multicenter study comparing the efficacy and safety of voxelotor (1500 mg and 900 mg daily) versus placebo for ≥24 weeks in patients aged 12 to 65 years with SCD. The primary endpoint is the percentage of patients with a Hb response at week 24, defined as a >1.0 g/dL increase in Hb. Secondary endpoints include change in markers associated with hemolysis: absolute reticulocyte count and percentage of reticulocytes, indirect bilirubin level, and lactate dehydrogenase (LDH) level. The per-protocol population was defined as those who completed the week 24 visit of the assigned treatment regimen and who did not initiate hydroxyurea treatment between baseline and week 24. Pharmacokinetic/pharmacodynamic modeling was used to correlate voxelotor exposure with Hb response and measures of hemolysis.
Results: A total of 229 patients (n=74, voxelotor 1500 mg; n=79, voxelotor 900 mg; n=76, placebo) were included in the per-protocol analysis. Among patients receiving voxelotor 1500 mg, all measures of hemolysis were consistently lower for those with changes in Hb of >1 g/dL compared with those with changes of ≤1 g/dL (Table 1). In the 900 mg group, percentage of reticulocytes, bilirubin, and LDH were lower for those with changes in Hb of >1 g/dL compared with those with changes of ≤1 g/dL; this pattern was not seen for absolute reticulocytes in this cohort. Generally, the degree of reduction in hemolysis markers was greater in the 1500 mg arm compared with the 900 mg arm.
Linear relationships between voxelotor exposure and Hb and LDH response were observed. In addition, saturable relationships between reticulocytes and bilirubin were also observed.
Conclusions: Among patients treated with voxelotor, those with Hb changes of >1.0 g/dL had the greatest reductions in the markers of hemolysis. In addition, patients with Hb changes of >1 g/dL and who received voxelotor 1500 mg had lower hemolytic markers than those who received voxelotor 900 mg, suggesting that exposure to a higher dose of voxelotor results in a greater decrease in hemolysis markers. Taken together, these results suggest that the mechanism by which voxelotor raises Hb is related to a reduction in hemolysis, which may modify the morbidity of SCD by improving hemolytic anemia.
Howard:Imara: Consultancy, Other: Travel grant; Global Blood Therapeutics: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel grant; Resonance Health: Other: Travel grant. Vichinsky:Global Blood Therapeutics: Consultancy; Agios: Research Funding; Pfizer: Research Funding. Knight-Madden:Global Blood Therapeutics: Research Funding; Nova Laboratories: Advisory Board on SCD 2017, Research Funding; Global Blood Therapeutics: Other: Sponsor of a conference held by Sickle Cell Unit in 2017; Addmedica: Other: Sponsor of a conference held by Sickle Cell Unit in 2017; BlueBird Bio: Other: Sponsor of a conference held by Sickle Cell Unit in 2017; Abbott Nutrition: Other: Sponsor of a conference held by Sickle Cell Unit in 2017; Abbot International: Other: Sponsor of a conference held by Sickle Cell Unit in 2017; Nova Laboratories: Other: Sponsor of a conference held by Sickle Cell Unit in 2017; Pfizer: Other: Advisory Board on SCD 2017. Tonda:Global Blood Therapeutics: Employment, Equity Ownership. Washington:Global Blood Therapeutics: Employment, Equity Ownership. Tong:Global Blood Therapeutics: Employment, Equity Ownership. Lehrer-Graiwer:Global Blood Therapeutics: Employment, Equity Ownership. Gordeuk:Emmaus: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Imara: Research Funding; Global Blood Therapeutics: Consultancy, Honoraria, Research Funding; CSL Behring: Consultancy, Honoraria, Research Funding; Ironwood: Research Funding; Inctye: Research Funding; Pfizer: Research Funding; Inctye: Research Funding; Novartis: Consultancy, Honoraria, Research Funding; CSL Behring: Consultancy, Honoraria, Research Funding; Modus Therapeutics: Consultancy, Honoraria; Global Blood Therapeutics: Consultancy, Honoraria, Research Funding; Emmaus: Consultancy, Honoraria; Ironwood: Research Funding; Modus Therapeutics: Consultancy, Honoraria; Imara: Research Funding; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal