Introduction
Chronic kidney disease (CKD) is a significant cause of morbidity and mortality in patients with sickle cell anemia (SCA). Albuminuria quantified by urinary albumin-to-creatinine ratio (ACR) is predictive of CKD and end-stage renal disease in other settings (non-SCA). As most sickle cell nephropathy studies are retrospective and cross-sectional, little is known about the natural progression of albuminuria in SCA and its correlation with glomerular filtration rate (GFR) decline and development of CKD.
Methods
We conducted a prospective, multicenter study (between 2009 and 2017) to investigate the longitudinal progression of sickle cell nephropathy (NCT02239016). Participants with SCA (HbSS or HbSb0 thalassemia) of all ages from 11 centers in the United States and the Caribbean were enrolled and provided urine and blood samples during routine clinic visits at steady-state. Urine ACR, cystatin C-estimated GFR (eGFR), and standard biomarkers of SCA and nephropathy in addition to kidney injury molecule (KIM-1) and N-acetyl-b-D-glucosaminidase (NAG) were followed longitudinally. Participants with albuminuria for ≥ 2 annual measurements were considered to have persistent albuminuria.
Results
A total of 303 participants with SCA were enrolled and followed for a median of 2 years. Participants were 1.6-64 years old (mean 21 years), and 46% were females. Participants provided annual samples (average 14.5-month interval between sample collections) and contributed to 644 patient-years on the study. 175 participants provided at least three annual samples and were included in a longitudinal analysis.
The prevalence of albuminuria (ACR>30mg/g) at baseline was 32% (97/303) of which 26% (80/303) had microalbuminuria (UACR 30-300 mg/g) and 6% (17/303) had macroalbuminuria (UACR>300 mg/g). At study entry, 45% of patients were prescribed hydroxyurea, and 20% received chronic transfusion therapy.
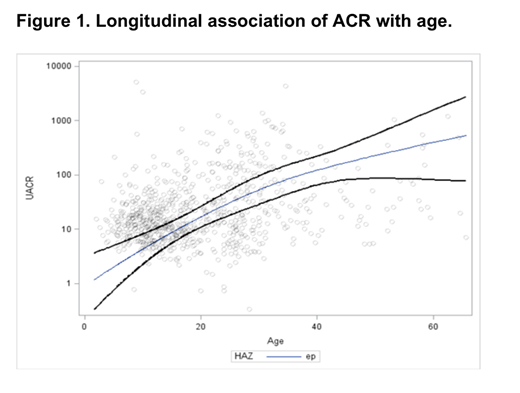
In univariate analysis, baseline ACR was significantly associated with older age (P<0.0001), sex (P=0.009), higher systolic and diastolic blood pressure (P<0.0001 and P=0.005), lower hemoglobin (P=0.01) and HbF (P=0.0005), higher bilirubin (P=0.001), and higher NAG (P<0.0001) and KIM-1 (P<0.0001). In a longitudinal multivariate analysis (years 0-3) that included the statistically significant variables from univariate analysis in addition to age-adjusted eGFR, only age (P=0.03), female sex (P=0.009), hemoglobin (P=0.01), bilirubin (P=0.002) and KIM-1 (P<0.0001) were significantly associated with ACR.
In participants who had at least 3 annual samples, a baseline ACR ≥100mg/g was predictive of persistent albuminuria (ACR>30mg/g for ≥2 annual measurements): 81% of participants with baseline ACR ≥100 mg/g had persistent albuminuria compared to 19% of participants with baseline ACR<100 mg/g. Participants with persistent albuminuria had significantly higher age, blood pressure, and serum creatinine, but were less likely to be on disease-modifying therapy (hydroxyurea or chronic transfusions), and had significantly lower HbF compared to those with non-persistent albuminuria.
eGFR correlated with age (P<0.0001) and persistent albuminuria (P=0.002), but not with baseline ACR. Participants with persistent albuminuria were also more likely to have a rapid decline in eGFR (a decline by >3 ml/min/1.73m2 per year) compared to those with non-persistent albuminuria (48% vs 31%, P=0.03).
Conclusion
In this longitudinal, prospective, multicenter study of sickle nephropathy, albuminuria was strongly associated with age and progressed over time (figure 1). Despite variability in spot urine ACR measurements, high baseline ACR ( ≥100mg/g) was associated with persistent albuminuria. Patients with persistent albuminuria were more likely to have rapid eGFR decline, a high-risk factor for CKD progression. Use of hydroxyurea and chronic transfusions was associated with less incidence of persistent albuminuria. Our results demonstrate that persistent albuminuria and high ACR at baseline predict kidney function decline in SCA. These findings show the feasibility of determining ACR and monitoring sickle nephropathy at routine clinic visits and have important implications for clinical decision-making and the design of future controlled therapeutic trials.
Saraf:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Research Funding. Quinn:Celgene: Membership on an entity's Board of Directors or advisory committees; Amgen: Other: Research Support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal