In this issue of Blood, Jones and colleagues challenge the belief that children with asymptomatic catheter-related thrombosis require anticoagulant treatment by demonstrating the low incidence of thrombus extension, embolization, or clinically significant postthrombotic syndrome in a natural history study of critically ill children requiring a central venous catheter (CVC).1
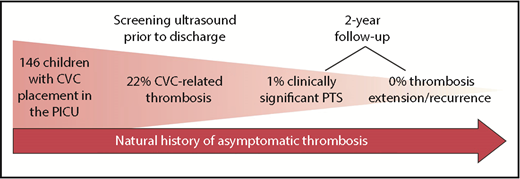
Natural history of asymptomatic CVC-RT in a population of pediatric intensive care unit (PICU) patients followed over 2 years. PTS, postthrombotic syndrome.
Natural history of asymptomatic CVC-RT in a population of pediatric intensive care unit (PICU) patients followed over 2 years. PTS, postthrombotic syndrome.
The management of asymptomatic thrombosis in a patient with a CVC has always been more controversial and variable than the management of symptomatic thrombosis. Fear of thrombus extension and/or embolization and concerns regarding the potential impact of the thrombus on CVC function and future vascular access are factors that lead to use of anticoagulation in patients with asymptomatic CVC-related thrombosis (CVC-RT). However, initiation of anticoagulation is no minor endeavor in this clinical setting. The potential risk of bleeding, particularly in critically ill children, must always be considered. Despite ongoing investigations of the use of direct oral anticoagulants in pediatrics, standard therapy at this time remains low-molecular-weight heparin, which requires twice-daily subcutaneous injections for patients and caregivers already coping with the substantial burden of acute and/or chronic disease. The most recent evidence-based guidelines, published by the American College of Chest Physicians in 2012, recommend treatment of CVC-RT with low-molecular-weight heparin for 6 to 12 weeks.2 However, without any information on the natural history of asymptomatic CVC-RT, it is impossible for physicians to properly weigh the risks and benefits of anticoagulation for these patients.
In this prospective cohort study, Jones and colleagues recruited children who were admitted to the pediatric intensive care unit and also required a CVC in the jugular or femoral vein. During their admission, all study participants underwent ultrasound of the extremity in which the CVC was placed. A unique and key strength of the study design as compared with previously published studies of CVC-RT is that the clinical team was blinded to the presence or absence of asymptomatic thrombosis, so patients did not receive anticoagulation therapy. Two years later, participants underwent a follow-up ultrasound as well as a standardized clinical assessment for postthrombotic syndrome using validated instruments. The authors found that the rate of CVC-RT at the time of initial ultrasound was fairly high in their patient population (∼1 in 5 patients developed thrombosis) despite the use of prophylactic unfractionated heparin in the majority of patients. However, clinically significant postthrombotic syndrome was reported in only 2 children, and 0 children experienced radiological thrombosis extension or clinical embolization (see figure).
Other major strengths of this study were that definitions of thrombosis and other clinical outcomes were detailed and identified a priori, and the investigators achieved a 73% retention rate of their cohort at the 2-year follow-up visit. This work represents collaboration between clinical investigators in hematology, cardiology, critical care, and radiology. A major barrier to the successful execution of clinical studies in pediatric thrombosis has been the fact that thrombosis is often a complication of nonhematologic diseases. Hematologists must therefore collaborate with other specialties in the design and implementation of clinical trials, and this team of multidisciplinary clinical scientists is an example of the teamwork critical to advancing science in pediatric thrombosis.
Important limitations of the study should also be highlighted. Due to the collaborations described above, the cohort was heavily weighted toward patients with congenital heart disease and/or postcardiac surgery. As a result, the study population skewed heavily toward younger ages. The median age was 12 months, and 23% of the cohort consisted of neonates. This age distribution is important because neonates and infants are at increased risk of CVC-RT due to differences in their hemostatic systems and the increased ratio of their CVC to vessel diameter.3 The young age of the population could also have impacted long-term outcomes, because infants are less likely than adolescents to develop postthrombotic syndrome.4 The generalizability of the results is also limited because all children in this study had untunneled short-term CVCs, which carry a different risk of thrombosis than tunneled catheters,5 and perhaps differences in long-term outcomes. Future studies will need to focus on differently aged high-risk populations for CVC-RT, such as adolescent trauma patients,6 as well as patients with different types of CVC, such as children and adolescents with acute lymphoblastic leukemia who typically have tunneled catheters in place.7
The work of Jones and colleagues will likely be a “game changer” in the management of asymptomatic pediatric thrombosis, because current guidelines (based on low-quality evidence) recommend anticoagulation for 6 to 12 weeks in such patients. This study provides high-quality evidence in a field that has been fraught with barriers to recruitment and retention in clinical research8 and supports the practice of observation alone in children with short-term CVCs and incidentally discovered CVC-RT.
Conflict-of-interest disclosure: S.O. receives research funding from Bristol Myers Squibb, has consulted for Pfizer, and has served on advisory boards for Shire and CSL Behring.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal