Abstract
Background: Recent advance in genetic analysis has revealed that many mutations are associated with the development, progression and/or prognosis of core-binding factor acute myeloid leukemia (CBF-AML). Although KIT mutation is the most frequently identified in CBF-AML, its prognostic relevance remains controversial. We conducted the prospective, multicenter cooperative study (JALSG CBF-AML209-KIT, UMIN Clinical Trials Registry UMIN000003434, http://www.umin.ac.jp/ctr/) to evaluate the prognostic impact of KIT mutation, the incidence and clinical relevance of the other gene mutations and prognostic impact of the minimal residual disease (MRD) in CBF-AML.
Methods: A total of 199 patients 16 to 64 years of age with newly diagnosed de novo AML were enrolled in this study if they had a RUNX1-RUNX1T1 or CBFB-MYH11 chimeric transcript and achieved complete remission within 2 courses of the standard induction therapies consisting of cytarabine and either daunorubicin or idarubicin. All patients were to be received 3 courses of high-dose cytarabine therapy (2 g/m2 by 3-hour infusion every 12 hours for 5 days) and no further chemotherapy until relapse. MRD level was evaluated in BM after the completion of the 3-course of consolidation therapy by the quantitation of RUNX1-RUNX1T or CBFB-MYH11 transcript in 112 patients. Target sequencing of 56 genes frequently identified in myeloid malignancies including exons 8, 10, 11 and 17 of the KIT gene were analyzed using the preserved DNA extracted from AML cells at diagnosis.
Results: A total of 68 KIT mutations were identified in 63 of 199 patients (31.7%); 42 of 132 (31.8%) and 21 of 67 (31.3%) patients with RUNX1-RUNX1T1 and CBFB-MYH11, respectively. Mutation in exon 17 was the most frequently identified (73.5%), followed by in exon 8 (20.6%) and in exon 10-11 (5.9%). Mutation in exon 8 was more frequent in AML with CBFB-MYH11 (37.5%) than that with RUNX1-RUNX1T1 (11.4%, P=0.014). Although mutation at N822 residue in exon 17 was identified in 13/44 (29.5%) KIT mutations of the patients with RUNX1-RUNX1T1, no patient with CBFB-MYH11 had this mutation (P=0.008); however, mutation at the D816 residue was equally identified in patients with RUNX1-RUNX1T1 (21/44, 47.7%) and CBFB-MYH11 (13/24, 54.1%). The median BM blast percentage of the KIT mutation positive-patients (73.5%) was significantly higher than that of negative-patients (53.8%, P<0.0001).
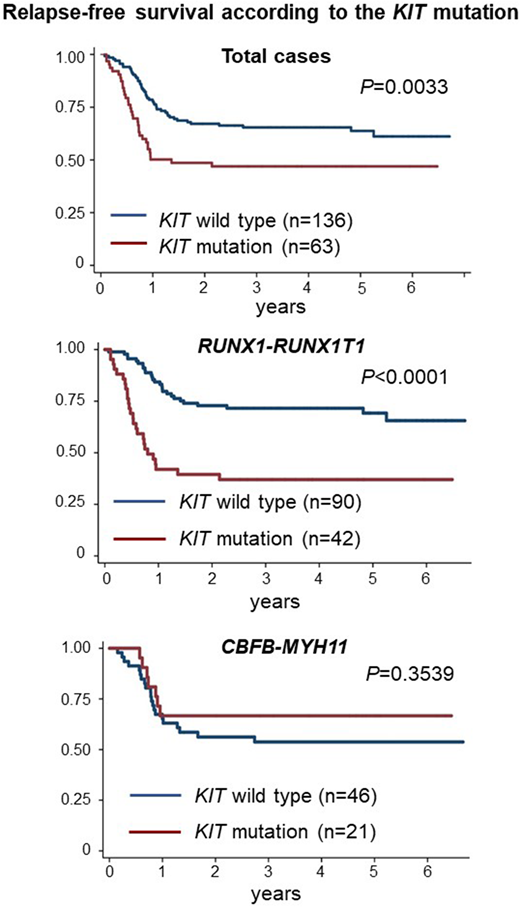
The median follow-up time was 1556 days (range, 356 - 2453 days). There was no significant difference in RFS and OS between the patients with RUNX1-RUNX1T1 and CBFB-MYH11. The 2-year RFS rate was 67.1% in KIT mutation negative-patients and 48.6% in positive-patients (P=0.0033). The 2-year OS rate was 91.0% in KIT mutation negative-patients and 74.6% in positive-patients (P=0.0005). In the patients with CBFB-MYH11, KIT mutations did not affect either RFS or OS. However, in the patients with RUNX1-RUNX1T1, KIT mutations had a strong impact both on 2-year RFS (72.8% vs. 39.5%, P<0.0001) and OS rates (89.7% vs. 63.5%, P<0.0001) in KIT mutation negative- and positive-patients, respectively. Among 3-types of KIT mutations, only the mutation in exon 17 had a worse prognostic impact on CBF-AML, which was also observed in the patients with RUNX1-RUNX1T1 (P<0.001), but not in those with CBFB-MYH11 (P=0.724). Furthermore, mutations at the D816 and N822 residues showed a worse prognostic impact (P<0.0001).
In addition to KIT mutations, NRAS (21.7%), FLT3 (12.1%) and ASXL2 (12.0%) genes were frequently identified in CBF-AML. ASXL1 mutation was a favorable factor for RFS in RUNX1-RUNX1T1 and NRAS mutation was a poor prognostic factor for RFS in CBFB-MYH11.
The 2-year RFS rate of the patients without MRD was significantly higher than that of those with MRD (81.3% vs. 55.4%, P=0.0075). Notably, the presence of the MRD was associated with worse RFS in the patients with CBFB-MYH11 (P=0.0144), but not in those with RUNX1-RUNX1T1 (P=0.1018).
Conclusions: This large-scale prospective study demonstrated that KIT mutation has an adverse effect for OS and RFS only on AML with RUNX1-RUNX1T1 but not on AML with CBFB-MYH11. Notably, we demonstrated that only mutations in the exon 17 of KIT gene had an adverse effect both on the RFS and OS of the patients with RUNX1-RUNX1T1, and the presence of MRD was a poor factor for RFS in AML with CBFB-MYH11.
Sawa:Celgene Corporation: Honoraria; Takeda Pharmaceutical Company Limited: Honoraria; Bristol-Myers Squibb: Honoraria; Novartis International AG: Honoraria; CHUGAI PHARMACEUTICAL CO., LTD.: Honoraria; Mundipharma K.K.: Honoraria. Dobashi:Pfizer Inc.: Research Funding; Chugai Pharmaceutical Co., Ltd.: Research Funding; Astellas Pharma Inc.: Research Funding; Kyowa Hakko Kirin Co. Ltd.: Research Funding; Zenyaku Kogyo Co., Ltd.: Research Funding; Eisai Co., Ltd.: Research Funding; Otsuka Pharmaceutical Co., Ltd.: Research Funding; Celgene Co.: Research Funding; Sysmex Co.: Research Funding. Asou:Kyowa Hakko Kirin Co., Ltd.: Speakers Bureau; Yakult Honsha Co., Ltd.: Speakers Bureau; SRL Inc.: Consultancy; Eisai Co., Ltd.: Research Funding; Asahi Kasei Pharma Co., Ltd.: Research Funding; Sumitomo Dainippon Pharma Co., Ltd.: Research Funding; Astellas Pharma Inc.: Research Funding; Chugai Pharmaceutical Co., Ltd.: Research Funding. Naoe:Pfizer Japan Inc.: Research Funding; Nippon Shinyaku Co., Ltd.: Research Funding; Otsuka Pharmaceutical Co., Ltd.: Research Funding; Astellas Pharma Inc.: Research Funding; Toyama Chemical Co., Ltd.: Research Funding; Fujifilm Corporation: Patents & Royalties, Research Funding. Kiyoi:Eisai Co., Ltd.: Research Funding; Kyowa Hakko Kirin Co., Ltd.: Research Funding; Sanofi K.K.: Research Funding; Bristol-Myers Squibb: Honoraria; Nippon Shinyaku Co., Ltd.: Research Funding; Astellas Pharma Inc.: Research Funding; Sumitomo Dainippon Pharma Co., Ltd.: Research Funding; Zenyaku Kogyo Co., Ltd.: Research Funding; Celgene Corporation: Research Funding; Takeda Pharmaceutical Co., Ltd.: Research Funding; Novartis Pharma K.K.: Research Funding; Phizer Japan Inc.: Research Funding; FUJIFILM Corporation: Research Funding; Otsuka Pharmaceutical Co., Ltd.: Research Funding; Chugai Pharmaceutical Co., Ltd.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal