Abstract
Introduction
Recently, progress has been made in the treatment of patients with higher risk myelodysplastic syndromes (HR MDS) and acute myeloid leukemia (AML). Nevertheless, patients failing hypomethylating agents (HMA) have a dismal prognosis and very limited treatment options. Targeting CD123 on leukemic stem cells (LSC) is one promising approach in MDS and AML. Talacotuzumab (TAL, JNJ-56022473) is an IgG1 monoclonal antibody targeting CD123 preferentially via antibody-dependent cellular cytotoxicity (ADCC) mediated by natural killer cells (NKs).
Aim
The SAMBA trial, a phase II study of the German and French MDS study groups within the EMSCO network assessed the overall hematological response rate after 3 months of single agent TAL treatment in AML or HR MDS patients failing hypomethylating agents (HMAs).
Methods
TAL was given IV at a dose of 9 mg/kg once every two weeks for a total of 6 infusions, responders received up to 20 additional infusions. After the first 3 months, overall hematological response rate (either CR, PR, marrow-CR, HI, SD) was evaluated by bone marrow biopsy. The study was accompanied by an immune monitoring via flow cytometric analysis to investigate the distribution of T- and NK cells in peripheral blood (PB) and bone marrow (BM) at the time of screening and during therapy in comparison with healthy, age-matched controls.
Results
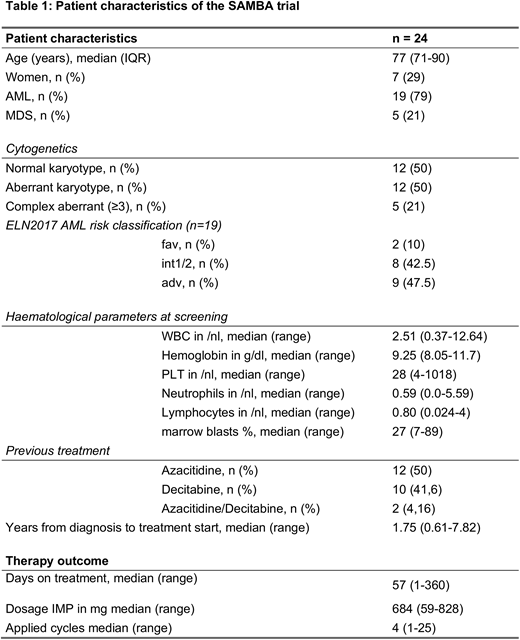
24 patients (19 AML and 5 HR MDS) with a median age of 77 (range 71-90) years, who either failed to achieve complete- (CR), partial response (PR), hematological improvement (HI) or relapsed after HMA therapy were included in the study. After TAL administration, 14 patients could be assessed for response after 4 infusions and 10 patients after 6 infusions. The overall response rate (ORR) was 20.8% including 1 complete remission (CRi), 1 patient with hematologic improvement (HI-E) and additionally 3 patients with disease stabilization. The median duration of response in these patients was 3 months (range 3-14 months). Two patients are still on treatment, one patient despite losing objective response (14 months) and one patient with disease stabilization (13 months). The median overall survival for the entire cohort of patients was 3.2 months (range 0.4-11.2 months). In 10 patients (41.6%), therapy with TAL resulted in grade 3/4 infusion related side effects (pneumonia, n=1; infusion-related reaction, n=8; septic shock, n=1).
Before treatment initiation, patients had lower levels of CD56dim NK-cells in PB (82% vs. 89% of NK-cells; p=0.069) expressing significantly more inhibiting NK-cell receptors like KIR2DL2 (8.8% vs. 3.2% of NK-cells; p<0.001) and less activating NK-cells receptors like NKG2D (95% vs. 99% of NK-cells; p<0.01) compared to healthy controls. Moreover, expression of PD-1 on lymphocytes and monocytes as well as their matching ligands PD-L1 and PD-L2 on blasts and monocytes in PB was significantly higher in patients compared to healthy controls (p<0.01), another evidence for an exhausted T-cell immune status in our patients prior to treatment initiation.
We could not detect any difference in NK-cell levels in responding patients compared to non-responders. Interestingly, pre-treatment expression (MFI and percentage) of CD123 on immature myeloid derived suppressor cells (iMDSC) was higher in responders than in non-responders (p<0.01). Anti-CD123 targeted therapy with TAL resulted in a decreased CD123+ MFI (4239 vs. 2910; p<0.01) on iMDSCs as well as lower levels of iMDSCs in PB and BM (p<0.05).Responding patients displayed a 10-fold reduction of CD123 MFI after 3 months of treatment (2565 vs. 236; p=0.06), indicating that the CD123 molecule on immature MDSCs is targeted effectively by TAL.
Conclusion
Single agent TAL has limited efficacy in patients with advanced myeloid malignancies failing HMA. Expression of CD123 on immature MDSCs might serve as a biomarker of response for future anti-CD123 targeted approaches.
Götze:Celgene: Honoraria, Research Funding; JAZZ Pharmaceuticals: Honoraria; Novartis: Honoraria; Takeda: Honoraria, Other: Travel aid ASH 2017. Krönke:Celgene: Honoraria. Middeke:Roche: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding. Fenaux:Celgene: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Jazz: Honoraria, Research Funding; Otsuka: Honoraria, Research Funding. Schlenk:Pfizer: Research Funding, Speakers Bureau. Ades:JAZZ: Honoraria; Takeda: Membership on an entity's Board of Directors or advisory committees; silent pharma: Consultancy; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Platzbecker:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal