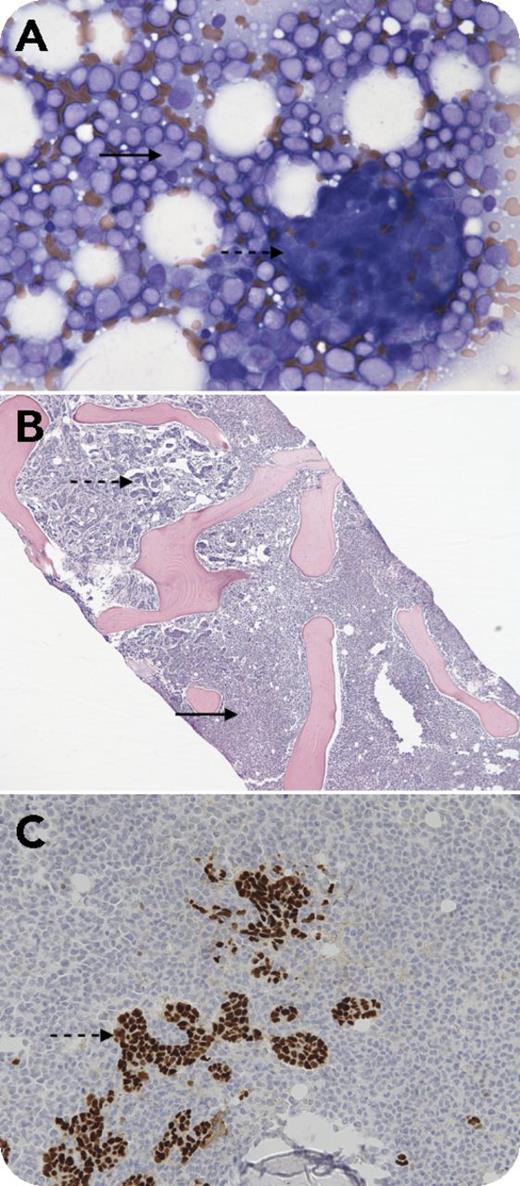
A 53-year-old woman was admitted with right thigh pain. She was diagnosed with estrogen receptor (ER)- and progesterone receptor (PR)-positive stage III adenocarcinoma of the left breast 3 years before. She was treated with lumpectomy and adjuvant doxorubicin and cyclophosphamide followed by paclitaxel and radiotherapy, but declined hormonal therapy. A right hip radiograph showed multiple lytic lesions, and positron emission tomography/computed tomography imaging confirmed widespread bony lesions. A complete blood count revealed a white blood cell count of 25 × 109/L with 20% blasts, a hemoglobin count of 11.1 g/dL, and a platelet count of 52 × 109/L. Bone marrow touch preparation (panel A; Wright's stain, original magnification ×400) and core biopsy (panel B; hematoxylin and eosin stain, original magnification ×40) were effaced by myeloblasts (solid arrows) and infiltrating adenocarcinoma arranged in clusters, ducts, and cords (dashed arrows) that were ER (panel C, dashed arrow; original magnification ×200) and PR positive and Her2 negative by immunohistochemistry. Cytogenetics revealed t(9;11)(p22;q23) and monosomy 7. Fluorescent in situ hybridization was positive for an MLL rearrangement. The patient was started on an aromatase inhibitor for her metastatic breast cancer and hypomethylating therapy for her acute myeloid leukemia (AML).
Rearrangements of the MLL (or KMT2A) gene are frequently seen in therapy-related AML after treatment with topoisomerase II inhibitors with a short latency of 2 to 3 years as compared with AML induced by alkylating agents, which has a latency of 5 to 7 years.
A 53-year-old woman was admitted with right thigh pain. She was diagnosed with estrogen receptor (ER)- and progesterone receptor (PR)-positive stage III adenocarcinoma of the left breast 3 years before. She was treated with lumpectomy and adjuvant doxorubicin and cyclophosphamide followed by paclitaxel and radiotherapy, but declined hormonal therapy. A right hip radiograph showed multiple lytic lesions, and positron emission tomography/computed tomography imaging confirmed widespread bony lesions. A complete blood count revealed a white blood cell count of 25 × 109/L with 20% blasts, a hemoglobin count of 11.1 g/dL, and a platelet count of 52 × 109/L. Bone marrow touch preparation (panel A; Wright's stain, original magnification ×400) and core biopsy (panel B; hematoxylin and eosin stain, original magnification ×40) were effaced by myeloblasts (solid arrows) and infiltrating adenocarcinoma arranged in clusters, ducts, and cords (dashed arrows) that were ER (panel C, dashed arrow; original magnification ×200) and PR positive and Her2 negative by immunohistochemistry. Cytogenetics revealed t(9;11)(p22;q23) and monosomy 7. Fluorescent in situ hybridization was positive for an MLL rearrangement. The patient was started on an aromatase inhibitor for her metastatic breast cancer and hypomethylating therapy for her acute myeloid leukemia (AML).
Rearrangements of the MLL (or KMT2A) gene are frequently seen in therapy-related AML after treatment with topoisomerase II inhibitors with a short latency of 2 to 3 years as compared with AML induced by alkylating agents, which has a latency of 5 to 7 years.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal