TO THE EDITOR:
Allogeneic hematopoietic stem-cell transplantation (ASCT) is curative treatment for patients with high-risk acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS), who otherwise have dismal outcomes.1-4 The TP53 gene is located in the 17p13 chromosomal region and is 1 of the major tumor suppressor genes, often inactivated by deletion and/or mutation in many tumors, including hematologic malignancies.5-8 TP53 mutations in AML and MDS are associated with significantly lower responses to standard chemotherapy and have emerged as a strong negative prognostic marker with poor treatment outcomes,6,8-15 including with ASCT.3,4,8,12-14
Here we hypothesized that outcomes of patients with TP53-mutated AML/MDS are not uniformly poor and aimed to identify prognostic factors for survival in patients with TP53-mutated AML/MDS undergoing ASCT.
A total of 83 consecutively treated patients with TP53-mutated AML or MDS who underwent their first ASCT at The University of Texas MD Anderson Cancer Center between February 2011 and March 2017 were analyzed. The median age at diagnosis was 60 years (range, 18-75 years); 38 patients (46%) were age >60 years. Ten patients (12%) had secondary AML/MDS; 82 patients (99%) had poor-risk cytogenetics at diagnosis. The median hematopoietic stem-cell transplantation comorbidity index (HCT-CI) was 4 (range, 0-9); Karnofsky performance status (KPS) was >80% in 56 patients (68%). Thirty-one patients (37%) were in first or second complete remission (CR1/2) at the time of transplantation. Conditioning regimens were busulfan based and melphalan based in 83% and 17%, respectively. Fifty-nine patients (71%) received myeloablative conditioning. Donors were HLA matched related (n = 27), matched unrelated (n = 41), haploidentical (n = 12), umbilical cord blood (n = 2), and antigen mismatched related (n = 1). Graft sources were bone marrow and peripheral blood in 32 (39%) and 49 (59%) patients, respectively. Thirteen patients received maintenance therapy with azacitidine (n = 11), decitabine (n = 1), or sorafinib (n = 1) post-transplantation. Twenty-one patients (25.3%) were alive at last follow-up, and 14 patients (16.9%) were disease free. The median follow-up for survivors was 12 months. The median overall survival (OS) was 8 months, with 1-year OS of 35% (95% confidence interval [CI], 25%-46%), and the median progression-free survival (PFS) was 5 months, with 1-year PFS of 25% (95% CI, 16%-35%). Nonrelapse mortality (NRM) and relapse at 1 year were 20% and 53%, respectively.
We evaluated predictors for NRM, relapse, OS, and PFS considering the following variables: age, HCT-CI of >4 vs ≤4, KPS of >80% vs ≤80%, disease status of CR1/2 vs other, conditioning regimen, donor type, cell source, secondary AML/MDS (yes vs no), and treatment-related AML/MDS (yes vs no), with azacitidine maintenance as a time-dependent variable. In multivariate analysis, factors associated with NRM were melphalan-based regimen (hazard ratio [HR], 6.5; 95% CI, 2.1-20; P = .001), KPS ≤80% (HR, 2.8; 95% CI, 0.96-8; P = .06), and treatment-related AML/MDS (HR, 4.2; 95% CI, 1.5-12; P = .007). None of the factors evaluated predicted for higher relapse rate, including remission status at transplantation. Independent factors that predicted better PFS were KPS >80% (HR, 2.1; 95% CI, 1.1-3.7; P = .02) and busulfan-based conditioning with a total area under the curve of 20 000 to 25 000 μmol/min (HR, 1.7; 95% CI, 0.96-3.0; P = .07), and factors associated with worse OS were HCT-CI >4 (HR, 3.9; 95% CI, 1.2-13; P = .03), KPS ≤80% (HR, 3.04; 95% CI, 1.6-5.9; P = .001), and disease not in CR1/2 (HR, 4.1; 95% CI, 1.5-11; P = .004).
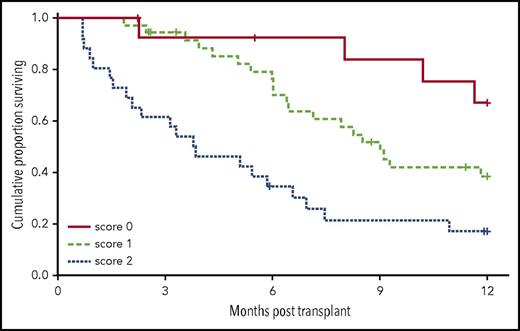
Because the HRs were comparable for these 3 significant factors, we assigned a score of 1 for each factor that predicted survival and evaluated OS based on the risk score. The 1-year OS rates for patients with a risk score of 0 (n = 14), 1 (n = 36), and ≥2 (n = 27) were 67% (HR, 0.2; 95% CI, 0.05-0.5; P = .001), 39% (HR, 0.4; 95% CI, 0.2-0.7; P = .002), and 17% (reference group), respectively (Figure 1). Azacitidine maintenance did not affect OS or PFS in these patients. Table 1 summarizes the treatment outcomes, and Table 2 summarizes the multivariate analysis.
Transplantation outcomes (n = 83)
| Outcome . | Result . |
|---|---|
| Median (range) follow-up for 21 survivors, mo | 12 (2.2-42) |
| N of patients progression free at last follow-up | 14 |
| Median OS, mo | 8 |
| Median PFS, mo | 5 |
| 1-y OS (95% CI), % | 35 (25-46) |
| 1-y PFS (95% CI), % | 25 (16-35) |
| 1-y NRM (95% CI), % | 20 (13-31) |
| 1-y relapse (95% CI), % | 53 (43-65) |
| Outcome . | Result . |
|---|---|
| Median (range) follow-up for 21 survivors, mo | 12 (2.2-42) |
| N of patients progression free at last follow-up | 14 |
| Median OS, mo | 8 |
| Median PFS, mo | 5 |
| 1-y OS (95% CI), % | 35 (25-46) |
| 1-y PFS (95% CI), % | 25 (16-35) |
| 1-y NRM (95% CI), % | 20 (13-31) |
| 1-y relapse (95% CI), % | 53 (43-65) |
Results of the multivariate analysis based on number of risk factors (n = 76)
| Risk score* . | N of patients . | N of failures . | HR . | 95% CI . | P . | 1-y PFS, % . |
|---|---|---|---|---|---|---|
| 0 | 22 | 12 | 0.3 | 0.1-0.6 | .003 | 40 |
| 1 | 42 | 30 | 0.5 | 0.2-0.9 | .03 | 25 |
| 2 | 12 | 11 | Ref | Ref | Ref | 8 |
| Risk score* . | N of patients . | N of failures . | HR . | 95% CI . | P . | 1-y PFS, % . |
|---|---|---|---|---|---|---|
| 0 | 22 | 12 | 0.3 | 0.1-0.6 | .003 | 40 |
| 1 | 42 | 30 | 0.5 | 0.2-0.9 | .03 | 25 |
| 2 | 12 | 11 | Ref | Ref | Ref | 8 |
Ref, reference.
1 score was assigned for each of the following factors: HCT-CI >4, KPS ≤80%, and disease not in CR1/2 at transplantation.
TP53 mutations have been previously identified as an independent adverse prognostic risk factor in patients with AML as well as those with MDS. Disease in this specific subset of patients is more resistant to standard chemotherapy and is incurable with chemotherapy alone.6,9,10,12 In our data set, patients were determined to have TP53 mutations by sequencing analysis. A majority of the patients showed a single TP53 mutation with no loss of 17p13 (n = 47 [58.75%] of 80); 17 (21.25%) of 80 patients had biallelic loss of TP53 by 2 TP53 mutations, and 16 (20%) had a combination of 17p13 deletion and TP53 mutation. In addition, we evaluated the correlations between cytogenetics and molecular data for these patients and found that 70 (85.3%) of 82 patients had complex karyotype (≥3 cytogenetic abnormalities), 56 (68.3%) of 82 had abnormalities of chromosome (CRS) 5, 49 (59.7%) of 82 had abnormalities of CRS 7, and 39 (47.5%) of 82 had both chromosomal abnormalities. Only 34 (41.5%) of 82 patients with TP53 mutations detected by molecular technique had abnormalities of CRS 17.
Although ASCT is the only potentially curative therapy for patients with TP53-mutated AML/MDS, mortality after transplantation remains high, with deaths attributable mostly to relapsed disease. Despite advances in ASCT, the overall prognosis of this group of patients remains poor.4,8,12,13 Predicting which patients will do better and most likely benefit from transplantation is thus a central challenge. Several studies have shown the ability of graft vs leukemia effect to overcome the poor prognosis in these patients after ASCT in CR1.3,4,7 A recent European Society for Blood and Marrow Transplantation analysis showed that ASCT for patients in CR1 with 17P abnormality led to a 2-year OS of 28% and leukemia-free survival of 24%. The 2-year NRM was 15%, and the 2-year relapse incidence was 61%.3 In patients with MDS analyzed in a Center for International Blood and Marrow Transplant Research study, the 3-year OS in 289 patients with TP53-mutated MDS was 20%, with a median OS of 0.7 years.8 In another study by Middeke et al,4 patients were risk stratified based on European Society for Blood and Marrow Transplantation risk score, integrating age, disease stage, time from diagnosis to transplantation, donor type, and donor-recipient sex combination. Patients with lower risk scores had significantly better OS and event-free survival. However, the 5-year probability of OS in the best risk group was only 20% (95% CI, 5-36).4
The 1-year NRM in our study was 20%, which is similar to the rates reported in previous studies. Not surprisingly, we found that patients who had high HCT-CI and poor PS at the time of transplantation had higher NRM. In addition, two thirds of all patients underwent transplantation beyond CR1/2, and more than half of these patients experienced disease relapse within 1 year post-transplantation, which could be an important contributing factor to the overall poor outcomes, as has been noted in multiple studies, reflecting biologic resistance to chemotherapy in these patients.
Although the OS at 1-year post-transplantation for the whole group was only 35%, we were able to identify a subgroup of patients with TP53-mutated AML/MDS who benefited the most from ASCT. Results from our study showed that patients with low HCT-CI, good PS, and disease in CR1/2 at the time of transplantation could achieve long-term survival. The 1-year OS in these patients was 67%. However, when ASCT was performed in patients with poor PS or multiple comorbidities or beyond CR1/2, the OS at 1 year was only 17%. Novel therapeutic strategies are needed to overcome the poor prognosis in these patients.
In addition, we also found that myeloablative doses of busulfan-based conditioning >20 000 μmol/min rather than lower doses seemed to be associated with better PFS. These results emphasize the importance of disease eradication by using a more intense conditioning chemotherapy before transplantation, especially in patients with good PS, whereas others might benefit from other novel therapeutic approaches.
Although provocative, these data should be interpreted with caution, because they are from a retrospective single-center experience with a limited number of patients. Larger retrospective studies and prospective validation of these findings are needed to confirm these findings and the utility of this prognostic score.
In conclusion, we were able to stratify the patients with TP53-mutated AML/MDS based on HCT-CI, PS, and disease status at transplantation and identified a subgroup of patients who did significantly better with this procedure. Patients with >1 risk factor in our analysis had poor long-term survival and should be considered for novel therapies before and/or after ASCT to reduce risk of relapse and prolong survival after transplantation. It remains to be seen if novel approaches to decrease relapse post-transplantation, such as the use of natural killer cells peritransplantation,16 will affect the survival outcomes of these patients.
Authorship
Contribution: S.O.C. designed the study, contributed to data collection and interpretation, and manuscript writing; A.C. wrote the initial draft of the manuscript; R.M.S. analyzed data and reviewed and approved the manuscript; J.C. and G.R. collected data and reviewed and approved the manuscript; K.P.P. and H.K. contributed to molecular data collection and interpretation and reviewed and approved the manuscript; A.R.S., B.V.R., and J.M.R.P. reviewed and approved the manuscript; and U.P., C.M.H., Q.B., R.M., G.A.-A., J.I., I.F.K., P.K., and R.E.C. contributed to treatment of patients and reviewed and approved the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Stefan O. Ciurea, Department of Stem Cell Transplantation and Cellular Therapy, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 423, Houston, TX 77030; e-mail: sciurea@mdanderson.org.