Abstract
Background: Chronic anemia is a significant problem affecting over 3 million Americans annually. Therapies are restricted to transfusion and Erythropoietin Stimulating Agents (ESA). There is a need for new approaches to treat chronic anemia. Immature erythroid progenitors are thought to be continuously produced and then permitted to survive and mature if there is sufficient erythropoietin (Epo) available. This model is elegant in that oxygen sensing within the kidney triggers Epo production so anemia can increase Epo and promote erythroid output. However, during homeostasis this model suggests that considerable energy is used to produce unneeded erythroid progenitors. We searched for independent control and compartmentalization of erythropoiesis that could couple early hematopoiesis to terminal erythroid commitment and maturation.
Methods: We previously found the proportion of bone marrow megakaryocytes (MKs) staining for active, signaling-competent TGFβ transiently increases during bone marrow regeneration after chemotherapy. To assess the functional role of Mk-TGFβ, we crossed murine strains harboring a floxed allele of TGFβ1 (TGFβ1Flox/Flox) littermate with a Mk-specific Cre deleter to generate mice with Mk-specific deletion of TGFβ1 (TGFβ1ΔMk/ΔMk). We analyzed hematopoiesis of these mice using high-dimensional flow cytometry, confocal immunofluorescent microscopy and in vitro and in vivo assays of hematopoietic function (Colony forming assays, and in vivo transplantation).
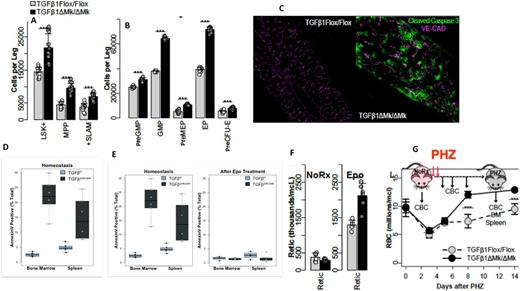
Results: Using validated, 9-color flow cytometry panels capable of quantifying hematopoietic stem cells (HSCs) and six other hematopoietic progenitor populations, we found that Mk-specific deletion of TGFβ1 leads to expansion of immature hematopoietic stem and progenitor cells (HSPCs) (Fig1A&B). Functional assays confirmed a more than three-fold increase in hematopoietic stem cells (HSCs) capable of serially-transplanting syngeneic recipients in the bone marrow (BM) of TGFβ1ΔMk/ΔMk mice compared to their TGFβ1Flox/Flox littermates. Expansion was associated with less quiescent (Go) HSCs implicating Mk-TGFβ in the control of HSC cell cycle entry. Similarly, in vitro colony forming cell assays and in vivo spleen colony forming assays confirmed expansion of functional progenitor cells in TGFβ1ΔMk/ΔMk mice. These results place Mk-TGFβ as a critical regulator of the size of the pool of immature HSPCs.
We found that the blood counts and total BM cellularity of TGFβ1ΔMk/ΔMk mice was normal despite the dramatic expansion of immature HSPCs. Using a combination of confocal immunofluorescence microscopy (cleaved caspase 3) (Fig1C) and flow cytometry (Annexin V and cleaved caspase 3) (Fig1D), we found ~10-fold greater apoptosis of mature precursor cells in TGFβ1ΔMk/ΔMk BM and spleens. Coincident with this, we found the number of Epo receptor (EpoR) expressing erythroid precursors to be dramatically increased. Indeed, apoptosis of erythroid precursors peaked as they transitioned from dual positive Kit+EpoR+ precursors to single positive cells expressing EpoR alone. Epo levels were normal in the serum of these mice. We reasoned that the excess, unneeded EpoR+ cells were not supported physiologic Epo levels but might respond to even small doses of exogenous Epo. Indeed, we found that the excess erythroid apoptosis could be rescued by administration of very low doses of Epo (Fig1E). Whereas TGFβ1Flox/Flox mice showed minimal reticulocytosis and no change in blood counts, TGFβ1ΔMk/ΔMk mice responded with exuberant reticulocytosis and raised RBC counts almost 10% within 6 days (Fig. 1F). Low dose Epo also rescued survival of Epo receptor positive erythroid precursors in the bone marrow, spleen and blood of TGFβ1ΔMk/ΔMk mice. TGFβ1ΔMk/ΔMk mice showed a similarly brisk and robust erythropoietic response during recovery from phenylhydrazine-induced hemolysis (Fig.1G). Exogenous TGFβ worsened BM apoptosis and caused anemia in treated mice. Pre-treatment of wild-type mice with a TGFβ signaling inhibitor sensitized mice to low dose Epo.
Conclusion: These results place megakaryocytic TGFβ1 as a gate-keeper that restricts the pool of immature HSPCs and couples immature hematopoiesis to the production of mature effector cells. This work promises new therapies for chronic anemias by combining TGFβ inhibitors to increase the outflow of immature progenitors with ESAs to support erythroid maturation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal