Abstract
The prognosis for patients with acute myeloid leukemia (AML) remains poor despite treatments. The need for new effective treatments in AML has led to the development of therapies that harness the immune system to attack the malignant cells. We have previously shown that neutrophil elastase (NE), proteinase 3 (P3) and cathepsin G (CG), serine proteases localized within azurophilic granules of myeloid cells, including myeloid leukemia, are immunotherapeutic targets for myeloid malignancies.
To determine whether other azurophilic granule components can be targeted in AML, we studied myeloperoxidase (MPO). MPO is maximally expressed at the promyelocytic stage of myeloid development and is later stored in the azurophilic granules of mature neutrophils. MPO function is implicated in the degradation and elimination of pathogenic bacteria during infection. MPO is also involved in the pathogenesis of certain autoimmune diseases such as granulomatosis with polyangiitis where it is targeted by humoral and cellular immunity. Importantly, MPO has been shown to be overexpressed in many types of leukemia, including CML, AML, and MDS, which suggests that it could be targeted if overexpression could break immune tolerance.
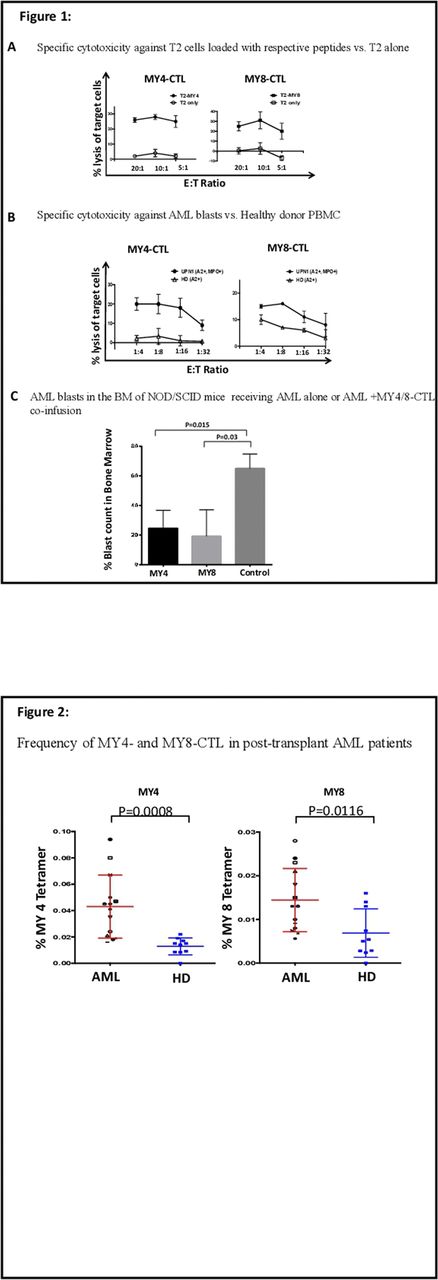
In this study, we identified two MPO-derived, HLA-A2-restricted peptides, MY4 and MY8, as novel leukemia-associate antigens (LAA). To identify these peptides, we first scanned the MPO sequence and screened potential peptides in silico against the binding motif of the HLA-A2 molecule. Ten peptides were predicted to have high binding affinity to HLA-A2 (Dissociation half-life over 100 min), and binding was confirmed by peptide-pulsed T2 binding assays with synthetic MPO peptides and flow cytometry. Next, we elicited cytotoxic T lymphocytes (CTL) from healthy HLA-A2+ donors and tested the resulting CTL for specificity and effector function in 4-hour cytotoxicity fluorescence assays against peptide-pulsed T2 cells and primary bone marrow cells from patients with refractory/relapsed AML (Fig 1 A+B). MY4- and MY8-specific cytotoxic T cells (CTL) are able to kill leukemia blasts while sparing healthy PBMCs from HLA-A2+ donors (Percentages of killing for MY4 CTL: 20, 20, 17, 8 vs. 2, 2, 1, 6 at 1:4,1:8,1:16:1:32 Effector: Target ratios respectively p<0.0001, Percentages of killing for MY8 CTL at the same E:T ratios: 15, 16,11,8 vs. 9,7,5,2 p=0.0023).
To examine potential in vivo activity against patient AML, we studied whether MPO-specific CTL could prevent or inhibit engraftment of primary AML in patient-derived mouse xenograft (PDX) models. Co-injection of MY4 or MY8-specific CTL with AML into sublethally irradiated NSG mice drastically reduced bone marrow tumor burden in vivo (Fig. 1C: 24%±6 for MY4 treated mice, n=4 vs. 65%±7 in the control group, n=2, p=0.01 and 19%±9 for MY8 treated mice, n=4 vs. 65%±7 in the control group n=2, p=0.03). Thus, these findings supported the hypothesis that MPO can be a LAA. To confirm whether MPO-specific immunity is linked to anti-leukemia immunity in patients, we studied post-allogeneic stem cell transplant (SCT) patients, where the graft-versus-leukemia (GVL) effect is critical for inducing and maintaining remission after SCT. We enumerated MPO-specific lymphocytes in the peripheral blood of patients post-SCT with MY4- and MY8/HLA-A2 tetramers. We found that MY4- and MY8-specific T cells are significantly increased in AML patients after SCT. These antigen specific T cells' frequency increased in post-transplant AML patients (n=14) as compared to healthy donors (n= 10) (Fig. 2: 0.043% ±0.006 vs. 0.01% ±0.002 of all peripheral -blood CD8 cells for MY4, p=0.0008 and 0.014% ±0.001 vs. 0.006% ±0.001 for MY8, p=0.01).
These result suggest that both MY4 and MY8 are immunogenic and MY4- and that MY8-specific CTL may play a role in targeting leukemia in patients after SCT. Thus, the discovery of MY4 and MY8 as novel LAAs paves the way for using these antigens in immunotherapy against myeloid leukemia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal