Key Points
HSCT represents an effective and definitive treatment of DADA2.
HSCT can cure the immunological, hematological, and vascular phenotype of DADA2 with 100% survival at median follow-up of 18 months.
Abstract
Deficiency of adenosine deaminase 2 (DADA2) is caused by biallelic deleterious mutations in CECR1. DADA2 results in variable autoinflammation and vasculopathy (recurrent fevers, livedo reticularis, polyarteritis nodosa, lacunar ischemic strokes, and intracranial hemorrhages), immunodeficiency and bone marrow failure. Tumor necrosis factor-α blockade is the treatment of choice for the autoinflammation and vascular manifestations. Hematopoietic stem cell transplantation (HSCT) represents a potential definitive treatment. We present a cohort of 14 patients from 6 countries who received HSCT for DADA2. Indication for HSCT was bone marrow dysfunction or immunodeficiency. Six of 14 patients had vasculitis pre-HSCT. The median age at HSCT was 7.5 years. Conditioning regimens were myeloablative (9) and reduced intensity (5). Donors were HLA-matched sibling (n = 1), HLA-matched unrelated (n = 9), HLA-mismatched unrelated (n = 3), and HLA haploidentical sibling (n = 1). All patients are alive and well with no new vascular events and resolution of hematological and immunological phenotype at a median follow-up of 18 months (range, 5 months to 13 years). Plasma ADA2 enzyme activity normalized in those tested post-HSCT (7/7), as early as day +14 (myeloid engraftment). Post-HSCT hematological autoimmunity (cytopenias) was reported in 4 patients, acute graft-versus-host disease grade 1 in 2, grade 2 in 3, and grade 3-4 in 1, and moderate chronic graft-versus-host disease in 1 patient. In conclusion, in 14 patients, HSCT was an effective and definitive treatment of DADA2.
Introduction
In 2014, 2 independent studies reported biallelic deleterious mutations in the cat eye chromosome region 1 gene (CECR1), encoding adenosine deaminase 2 (ADA2), as the cause of a new and rare autoinflammatory condition, named human deficiency of ADA2 syndrome (DADA2) (OMIM #615688).1,2 In the initial reports, DADA2 was hallmarked by recurrent episodes of fever with elevation of acute-phase reactants and vasculopathy ranging from early-onset cutaneous livedo reticularis, Raynaud phenomenon, and polyarteritis to life-threatening intracranial vasculopathy with lacunar strokes and hemorrhages.3,4 Bone marrow dysfunction, which may include pure red cell aplasia (PRCA), Diamond-Blackfan–like anemia, thrombocytopenia, and neutropenia, is now recognized as an equally important manifestation.5,6 In addition, immunodeficiency can be found with hypogammaglobulinemia (especially immunoglobulin M [IgM]) as well as disturbances in the T-cell compartment.7 Inflammatory bowel disease, reminiscent of the bowel involvement found in patients with common variable immunodeficiency (devoid of plasma cells), can also be found. Eight of the nearly 100 DADA2 patients (8%) reported to date in the literature are deceased.1,2,8,9 The most common reason of death was stroke (in 4/8 patients). The diagnosis of DADA2 is based on the measurement of low/absent plasma ADA2 enzymatic activity and on the identification of biallelic loss-of-function mutations in CECR1, which is located within chromosome 22q11. Patients with homozygous deletions encompassing the CECR1 locus on 22q11 show the same phenotype. Also, absent plasma ADA2 enzymatic activity has been described in singular patients with monoallelic mutations in CECR1. It is unclear at this point whether in these cases a second (cryptic) mutation is present on the other allele, in an intron, in the promoter region, or rather in a different gene affecting ADA2 expression. Alternatively, copy number variations affecting the CECR1 locus may have been missed.
In humans, 2 ADA proteins have been described: ADA1 and ADA2. Deficiency of ADA1, encoded by the ADA gene on chromosome 20q, causes severe combined immunodeficiency owing to profound depletion of T, B, and NK lymphocytes, which normally show high expression of ADA1. In these patients, plasma levels of adenosine and deoxyadenosine are elevated, and their red cells show a marked accumulation of 2′-deoxyadenosine triphosphate (dATP, derived from deoxyadenosine). Lymphopenia has been attributed primarily to dATP pool expansion, which blocks DNA synthesis and induces apoptosis in immature lymphoid cells. Aberrant signaling via receptors for adenosine may contribute to nonimmunologic features that occur in some ADA1-deficient patients. In contrast to ADA1, ADA2 is primarily expressed by myeloid cells and mainly secreted in plasma by monocytes.10 The function of ADA2 in cellular pathways is still enigmatic, and its absence in mice has hampered investigation of pathogenic mechanisms. However, where studied, the levels of adenosine and deoxyadenosine in plasma, and of dATP in red cells, have not been elevated in DADA2.1,2 It has been postulated that ADA2 is an adenosine deaminase–related growth factor.11 In vitro studies suggest that ADA2 secreted from monocytes acts as an autocrine factor to stimulate their differentiation into macrophages and dendritic cells.12 ADA2 may play a role in maintaining the balance between M1 and M2 macrophages, with ADA2 deficiency leading to an M1 proinflammatory phenotype as reviewed by Martinon and Aksentijevich.13 A mixed neutrophil and type I interferon signature was observed in 2 ADA2-deficient patients.14 This correlated with increased levels of proinflammatory cytokines such as interleukin-6 in the plasma of ADA2-deficient patients in 2 studies and with the vasculitis seen in patients with DADA2. Despite CECR1 not being expressed in the endothelium, deficiency of ADA2 leads to endothelial instability as also shown in the zebrafish model and in coculture systems of endothelial cells.1,2
Medical management of patients with DADA2 is challenging. None of the commonly used immunosuppressive drugs have been particularly effective in controlling disease manifestations. Etanercept in particular or anti–tumor necrosis factor agents have shown promise in the management of the inflammatory syndrome and vasculitis.7,15 However, at least etanercept does not appear to reverse the hematological phenotype (Polina Stepensky, unpublished observation, n = 5). Soon after the first description of DADA2, hematopoietic stem cell transplantation (HSCT) was reported to result in a rapid and sustained immune reconstitution and resolution of the systemic inflammation.16,17 Indeed, given that monocytes are the main cellular source for ADA2, there is a strong rationale for HSCT as a potential cure. Additional patient case reports have since confirmed these findings.6,18-20 The aim of the present study is to better define the role for HSCT as a potential cure for DADA2. We report the results of a multinational cohort study of 14 patients with proven DADA2 who underwent HSCT, including the previously reported cases. All are alive, well, and cured.
Patients and methods
We conducted an international cohort study on patients with DADA2 via the European Group for Blood and Marrow Transplantation, European Society for Immunodeficiencies, Primary Immunodeficiency Transplant Consortium, and Center for International Blood and Marrow Transplant Research. Data collection started after the Inaugural International Conference on Deficiency of ADA2 hosted by the DADA2 Foundation and held in Bethesda, MD, on November 11, 2016. Criteria for patient inclusion into the study were: (1) diagnostic findings consistent with DADA2 and confirmed by genetic testing and/or (2) diagnostic findings consistent with DADA2 and absent plasma ADA2 activity and (3) HSCT performed with a follow-up time more than 5 months after HSCT. A questionnaire was completed by participating physicians. Data were obtained in accordance with the Declaration of Helsinki. All patients or their guardians gave written informed consent for data collection. The study was approved by the Ethical Committee of the University Hospitals Leuven. Neutrophil engraftment was defined as the first of 3 consecutive days when the absolute neutrophil count was ≥0.5 × 109/L, platelet engraftment defined as the first of 7 days without a platelet transfusion that the platelet count was ≥20 × 109/L, and full donor chimerism was defined as ≥95% of leukocytes being of donor origin in peripheral blood or bone marrow samples. The diagnosis and grading of acute and chronic graft-versus-host disease (GVHD) were defined according to international standard criteria.
Results
We received complete data sets for 14 DADA2 patients transplanted between 2000 and 2016. Patients received treatment in 11 different centers in 6 countries in Europe and North America. Five patients were reported previously.16-21 The male/female ratio was 8/6. The median age at initial presentation was 1.5 years (range, birth to 16 years). The median age at genetic diagnosis was 10 years (range, 2-25 years) (Table 1). The diagnosis of DADA2 was confirmed at the molecular level by demonstration of biallelic deleterious CECR1 mutations in all patients. Plasma ADA2 enzyme activity before HSCT was low in 6/6 patients tested (Table 2). Six of 14 patients had vasculitis before HSCT, 3 of whom had intracranial hemorrhage. All patients except 1 had received at least 1 line of immunosuppressive treatment before HSCT. Hematological manifestations were prominent in this cohort, with PRCA documented in 7/14 patients, neutropenia in 6/14, immunomediated thrombocytopenia (ITP) in 2/14 and pancytopenia in 3/14 at presentation. Low IgG was present in 7/10, low IgA in 7/10, and low IgM in 7/10 measured. Seven of 14 patients had recurrent infections, of whom 3/7 especially viral infections. Ten of 14 patients were on immunoglobulin substitution before HSCT and only 2 continue to require replacement post-HSCT (both less than a year post-HSCT). Splenomegaly was present in 11/14 patients.
Demographic and clinical features of the 14 DADA2 patients before HSCT
| Patient ID . | Sex/ethnicity . | Age at disease onset (y) . | Age at genetic diagnosis (y) . | DADA2 clinical manifestations . | CD4, CD8, CD19, CD56 (n × 106/L) . | IgG (mg/dL) . | IgA (mg/dL) . | IgM (mg/dL) . | Previous treatment . | Reference . |
|---|---|---|---|---|---|---|---|---|---|---|
| P001 | M, white | 3 | 4 | PRCA, HSM, alopecia, strabismus, recurrent fevers, aphthous ulcers | 814, 459, 104, 60 | 605 | 40 | <6 | Prednisone, MMF, sirolimus, CsA | 6, 21 |
| P002 | F, Hispanic | 7 | 21 | Recurrent infections, ID | 361, 262, 0, 32 | NA | NA | NA | Prednisone | 20 |
| P003 | F, white | 7 | 11 | Splenomegaly, ICH, livedo, arthritis | 528, 211, 26, 30 | NA | NA | NA | Infliximab | |
| P004 | F, white | 1 | 9 | Pancytopenia, stroke, ICH, vasculitis, arthritis, HSM, HTN, CMP, ID | 273, 222, 23, 29 | 354 | 34 | 9 | Prednisone, etanercept, anakinra, azathioprine | 19 |
| P005 | M, white | 0 | 2 | PRCA, LNP, HSM, recurrent infections | 1763, 1037, 415, 104 | 426 | <8 | <6 | Prednisone | |
| P006 | F, white | 14 | 15 | PRCA, neutropenia | 441, 276, 43, 35 | 499 | 11 | 15 | Prednisone | |
| P007 | M, white | 0.5 | 13 | PRCA, neutropenia, SAA, HSM, livedo, IDDM, GHD | NA | 360 | 60 | 30 | None | 17 |
| P008* | M, white | 0.5 | 5 | PRCA, pancytopenia, splenomegaly, recurrent infections, LNP | 653, 93, 11, 0.5 | 997 | 2.4 | 7 | Prednisone, sirolimus, tacrolimus | 16, 18 |
| P009* | M, white | 0.4 | 4 | Anemia, neutropenia, HSM, LNP, IBD, SAH, TIA, recurrent infections | 599, 278, 228, 147 | 436 | 17 | 54 | Prednisone, azathioprine, sirolimus, etanercept | |
| P010 | M, white | 2 | 22 | Anemia, lymphopenia, HSM, Livedo, ICH, HTN, optic nerve atrophy, PAN | 50, 50, 1, 10 | 465 | 47 | 17 | Prednisone, azathioprine, infliximab | |
| P011 | F, white | 2.5 | 4 | PRCA, vasculitis, pancytopenia, epilepsy, HSM, aphthous ulcers | 386, 257, 237, 41 | 1000 | 2.4 | 74 | Prednisone | |
| P012 | F, white | 16 | 25 | ITP, HSM, lymphoproliferation, recurrent infections, lung granuloma | 1670, 1721, 106, 101 | NA | NA | NA | Prednisone, ATG | |
| P013 | M, white | 0.3 | 9 | PRCA, neutropenia, splenomegaly, IBD, recurrent fevers, aphthous ulcers | 607, 781, 685, 90 | 290 | 119 | 9 | Prednisone, anakinra | |
| P014 | M, Hispanic | 0 | 18 | PRCA, hepatopathy, aphthous ulcers | NA | NA | NA | NA | Prednisone |
| Patient ID . | Sex/ethnicity . | Age at disease onset (y) . | Age at genetic diagnosis (y) . | DADA2 clinical manifestations . | CD4, CD8, CD19, CD56 (n × 106/L) . | IgG (mg/dL) . | IgA (mg/dL) . | IgM (mg/dL) . | Previous treatment . | Reference . |
|---|---|---|---|---|---|---|---|---|---|---|
| P001 | M, white | 3 | 4 | PRCA, HSM, alopecia, strabismus, recurrent fevers, aphthous ulcers | 814, 459, 104, 60 | 605 | 40 | <6 | Prednisone, MMF, sirolimus, CsA | 6, 21 |
| P002 | F, Hispanic | 7 | 21 | Recurrent infections, ID | 361, 262, 0, 32 | NA | NA | NA | Prednisone | 20 |
| P003 | F, white | 7 | 11 | Splenomegaly, ICH, livedo, arthritis | 528, 211, 26, 30 | NA | NA | NA | Infliximab | |
| P004 | F, white | 1 | 9 | Pancytopenia, stroke, ICH, vasculitis, arthritis, HSM, HTN, CMP, ID | 273, 222, 23, 29 | 354 | 34 | 9 | Prednisone, etanercept, anakinra, azathioprine | 19 |
| P005 | M, white | 0 | 2 | PRCA, LNP, HSM, recurrent infections | 1763, 1037, 415, 104 | 426 | <8 | <6 | Prednisone | |
| P006 | F, white | 14 | 15 | PRCA, neutropenia | 441, 276, 43, 35 | 499 | 11 | 15 | Prednisone | |
| P007 | M, white | 0.5 | 13 | PRCA, neutropenia, SAA, HSM, livedo, IDDM, GHD | NA | 360 | 60 | 30 | None | 17 |
| P008* | M, white | 0.5 | 5 | PRCA, pancytopenia, splenomegaly, recurrent infections, LNP | 653, 93, 11, 0.5 | 997 | 2.4 | 7 | Prednisone, sirolimus, tacrolimus | 16, 18 |
| P009* | M, white | 0.4 | 4 | Anemia, neutropenia, HSM, LNP, IBD, SAH, TIA, recurrent infections | 599, 278, 228, 147 | 436 | 17 | 54 | Prednisone, azathioprine, sirolimus, etanercept | |
| P010 | M, white | 2 | 22 | Anemia, lymphopenia, HSM, Livedo, ICH, HTN, optic nerve atrophy, PAN | 50, 50, 1, 10 | 465 | 47 | 17 | Prednisone, azathioprine, infliximab | |
| P011 | F, white | 2.5 | 4 | PRCA, vasculitis, pancytopenia, epilepsy, HSM, aphthous ulcers | 386, 257, 237, 41 | 1000 | 2.4 | 74 | Prednisone | |
| P012 | F, white | 16 | 25 | ITP, HSM, lymphoproliferation, recurrent infections, lung granuloma | 1670, 1721, 106, 101 | NA | NA | NA | Prednisone, ATG | |
| P013 | M, white | 0.3 | 9 | PRCA, neutropenia, splenomegaly, IBD, recurrent fevers, aphthous ulcers | 607, 781, 685, 90 | 290 | 119 | 9 | Prednisone, anakinra | |
| P014 | M, Hispanic | 0 | 18 | PRCA, hepatopathy, aphthous ulcers | NA | NA | NA | NA | Prednisone |
Bold font indicates low values for age.
ATG, antithymocyte globulin; CMP, cardiomyopathy; CsA, cyclosporine A; F, female; GHD, growth hormone deficiency; HSM, hepatosplenomegaly; HTN, hypertension; ICH, intracranial hemorrhage; IBD, inflammatory bowel disease; ID, immunodeficiency; IDDM, insulin dependent diabetes mellitus; LNP, lymphadenopathy; M, male; MMF, mycophenolate mofetil; NA, not available; PAN, polyarteritis nodosa; SAH: subarachnoid hemorrhage; TIA: transient ischemic attack.
Siblings.
Genetic and biochemical basis for diagnosis of the 14 DADA2 patients
| Patient ID . | CECR1 allele 1 . | CECR1 allele 2 . | ADA2 activity pre-HSCT . | ADA2 activity post-HSCT . |
|---|---|---|---|---|
| P001 | c.1110C>A (p.N370K) | c.1072G>A (p.G358R) | 0.6* | 19.7 at 1 y* |
| P002 | c.794C>G (p.S265X) | c.794C>G (p.S265X) | 0.0* | 10.8 at 1 y* |
| P003 | c.660C>A (p.Y220X) | c.660C>A (p.Y220X) | 2.5† | NA |
| P004 | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | 0.8* | 7.0 at 1 y* |
| P005 | c.144delG (p.R49fs) | c.506G>A (p.R169Q) | NA | NA |
| P006 | c.144dupG (p.R49fs) | c.506G>A (p.R169Q) | NA | NA |
| P007 | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | NA | 15.3 at 3 mo* |
| P008‡ | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | NA | 22.07* |
| P009‡ | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | 0.11* | NA |
| P010 | c.506C>T (p.R169Q) | c.2T>C (p.M1T) | NA | NA |
| P011 | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | NA | NA |
| P012 | c.140G>T (p.G47V) | c.336C>G (p.H112Q) | NA | NA |
| P013 | c.144del (p.R49fs) | c.47+2T>C (splice site) | 0.2* | 11.7* |
| P014 | c.506G>A (p.R169Q) | c.1072G>A (p.G358R) | NA | 22.3* |
| Patient ID . | CECR1 allele 1 . | CECR1 allele 2 . | ADA2 activity pre-HSCT . | ADA2 activity post-HSCT . |
|---|---|---|---|---|
| P001 | c.1110C>A (p.N370K) | c.1072G>A (p.G358R) | 0.6* | 19.7 at 1 y* |
| P002 | c.794C>G (p.S265X) | c.794C>G (p.S265X) | 0.0* | 10.8 at 1 y* |
| P003 | c.660C>A (p.Y220X) | c.660C>A (p.Y220X) | 2.5† | NA |
| P004 | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | 0.8* | 7.0 at 1 y* |
| P005 | c.144delG (p.R49fs) | c.506G>A (p.R169Q) | NA | NA |
| P006 | c.144dupG (p.R49fs) | c.506G>A (p.R169Q) | NA | NA |
| P007 | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | NA | 15.3 at 3 mo* |
| P008‡ | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | NA | 22.07* |
| P009‡ | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | 0.11* | NA |
| P010 | c.506C>T (p.R169Q) | c.2T>C (p.M1T) | NA | NA |
| P011 | c.506G>A (p.R169Q) | c.506G>A (p.R169Q) | NA | NA |
| P012 | c.140G>T (p.G47V) | c.336C>G (p.H112Q) | NA | NA |
| P013 | c.144del (p.R49fs) | c.47+2T>C (splice site) | 0.2* | 11.7* |
| P014 | c.506G>A (p.R169Q) | c.1072G>A (p.G358R) | NA | 22.3* |
Plasma ADA2 (mU/mL): healthy controls (n = 20 + pooled normal plasma), 14.2 ± 5.2 (4.8-27.2); DADA2 patients (n = 25), 0.4 ± 0.5 (0.02-1.7).
Dried plasma spots ADA2 (mU/g protein): healthy controls (n = 39), 130.5 ± 49.8 (58-271); DADA2 patients (n = 40), 4.4 ± 4.3 (0.04-17.2).
Siblings.
The median age at HSCT was 7.5 years (range, 2-23 years). Overall survival of patients undergoing HSCT was 100% (14/14 patients alive). Six of 14 patients had received HSCT before description of the condition in 2014. Indications for HSCT were bone marrow dysfunction (neutropenia, PRCA, thrombocytopenia) and/or immunodeficiency (hypogammaglobulinemia with recurrent infections) (Table 3). A total of 20 HSCT procedures were performed for 14 patients: 2 patients required a second transplant for engraftment failure because of use of apparently healthy sibling donors who later were discovered to carry the deleterious CECR1 mutations and be ADA2 deficient. They received salvage HSCT from matched unrelated donors. One patient required a second HSCT for graft failure. Another patient required a boost because of insufficient stem cell dose at first transplant. Yet another patient originally received myeloablative conditioning but required 2 unconditioned boosts following a drop in whole blood chimerism to 30%. This coincided with a decline of plasma ADA2 enzyme activity to pretransplant levels and a new presentation of autoimmune PRCA followed by agranulocytosis. Regimens were different across transplant centers. Nine patients received myeloablative conditioning and 5 received a reduced intensity regimen. The most commonly used regimen (in 5 patients) was treosulfan/fludarabine ± thiotepa with ATG or alemtuzumab. Serotherapy was used in 12/14 patients: ATG in 4 and alemtuzumab in 8 patients. Bone marrow was the source of stem cells in 10 grafts and peripheral blood stem cells in 4 grafts. Donors were matched sibling (n = 1), haploidentical sibling (n = 1), 10/10 matched unrelated (n = 9), and mismatched unrelated (n = 3) for the final curative transplant procedures. Methotrexate associated with a calcineurin inhibitor was the prophylactic regimen for GVHD in 9/14 patients (Table 3). All patients received antimicrobial and GVHD prophylaxis at the discretion of the transplant physician/center.
Transplant data and post-HSCT complications for the 14 DADA2 patients
| Patient ID . | Year of HSCT . | Age at HCT (y)/sex . | Indication of HSCT . | HLA match/graft source . | Conditioning . | GVHD prophylaxis . | aGVHD/grade . | cGVHD . | Viral comp . | Autoimmune comp . | Last chimerism . | Last follow-up (mo) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P001 | 2016 | 4/M | PRCA, neutropenia | 10/10 MUD BM | Flu/mel/alem (RIC) | MTX/tacro | No | No | EBV/HHV6 | ITP | 1 y 98% | 14 |
| P002 | 2013 | 20/F | Neutropenia | 5/10 haplo BM (boost for low CD34 dose, 0.5 × 106/kg) | Flu/bu/cy/TBI200 | Tacro/MMF/PTCy | No | No | None | None | 3 y 100% | 41 |
| P003 | 2016 | 11/F | Pancytopenia, autoimmunity | 10/10 MUD PB | Flu/treo/TT/ATG | MTX/CsA | Skin grade 1 | No | Adeno/HHV6, BK | None | 6 mo 100% | 12 |
| P004 | 2012 | 8/F | Pancytopenia | 9/10 MMUD BM | Flu/treo/alem | MTX/CsA | No | No | Adeno/VZV | None | 5 y 100% | 60 |
| P005 | 2016 | 2/M | PRCA, recurrent CMV | 10/10 MUD BM | Flu/treo/TT/ATG | MTX/CsA | Skin grade 2 | No | Adeno | None | 6 mo 100% | 12 |
| P006 | 2016 | 16/F | PRCA, neutropenia | 9/10 MMUD PB (second HSCT for GF) | Flu/TT/ATG (RIC) | MTX/CsA | No | No | BK/CMV | None | 1 mo 100% | 4 |
| P007 | 2003 | 4/M | Refractory SAA | 10/10 MUD BM (first HSCT from affected MSD) | Flu/TBI/alem (RIC) | MTX/CsA | No | No | Adeno | None | 3 y 100% | 161 |
| P008* | 2009 | 3/M | PRCA, neutropenia | MSD BM | Bu/cy | MMF/CsA | Colon grade 3-4 | No | VZV | ITP | 3 y >95% | 76 |
| P009* | 2016 | 5/M | Recurrent TIA, immunodeficiency | 10/10 MUD PB (2 boosts for declining chimerism) | Flu/treo/alem | MMF/CsA | Skin grade 1 | No | Adeno/HSV1/BK | PRCA, neutropenia | 1 y >95% | 15 |
| P010 | 2016 | 23/M | Severe lymphopenia, hypogammaglobulinemia | 10/10 MUD BM | Flu/bu/alem | MTX/CsA | No | No | None | None | 6 mo >95% | 11 |
| P011 | 2016 | 5/F | PRCA, neutropenia | 10/10 MUD BM | Flu/treo/TT/alem | MMF/CsA | Skin grade 1 | No | CMV, EBV | None | 6 mo 100% | 10 |
| P012 | 2014 | 23/F | Severe neutropenia | 10/10 MUD BM | Flu/mel/alem (RIC) | Prednisone/CsA | No | No | None | None | 2 y 98% | 39 |
| P013 | 2015 | 7/M | PRCA | 10/10 MUD BM | Bu/cy/ATG | MTX/CsA | No | No | None | None | 1 y 100% | 21 |
| P014 | 2007 | 9/M | PRCA | MMUD PB (first HSCT from affected MSD) | Flu/TBI450/alem (RIC) | MTX/CsA | Skin grade 2 | Skin + liver moderate | CMV/adeno/BK | AIHA | 3 y 95% | 117 |
| Patient ID . | Year of HSCT . | Age at HCT (y)/sex . | Indication of HSCT . | HLA match/graft source . | Conditioning . | GVHD prophylaxis . | aGVHD/grade . | cGVHD . | Viral comp . | Autoimmune comp . | Last chimerism . | Last follow-up (mo) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P001 | 2016 | 4/M | PRCA, neutropenia | 10/10 MUD BM | Flu/mel/alem (RIC) | MTX/tacro | No | No | EBV/HHV6 | ITP | 1 y 98% | 14 |
| P002 | 2013 | 20/F | Neutropenia | 5/10 haplo BM (boost for low CD34 dose, 0.5 × 106/kg) | Flu/bu/cy/TBI200 | Tacro/MMF/PTCy | No | No | None | None | 3 y 100% | 41 |
| P003 | 2016 | 11/F | Pancytopenia, autoimmunity | 10/10 MUD PB | Flu/treo/TT/ATG | MTX/CsA | Skin grade 1 | No | Adeno/HHV6, BK | None | 6 mo 100% | 12 |
| P004 | 2012 | 8/F | Pancytopenia | 9/10 MMUD BM | Flu/treo/alem | MTX/CsA | No | No | Adeno/VZV | None | 5 y 100% | 60 |
| P005 | 2016 | 2/M | PRCA, recurrent CMV | 10/10 MUD BM | Flu/treo/TT/ATG | MTX/CsA | Skin grade 2 | No | Adeno | None | 6 mo 100% | 12 |
| P006 | 2016 | 16/F | PRCA, neutropenia | 9/10 MMUD PB (second HSCT for GF) | Flu/TT/ATG (RIC) | MTX/CsA | No | No | BK/CMV | None | 1 mo 100% | 4 |
| P007 | 2003 | 4/M | Refractory SAA | 10/10 MUD BM (first HSCT from affected MSD) | Flu/TBI/alem (RIC) | MTX/CsA | No | No | Adeno | None | 3 y 100% | 161 |
| P008* | 2009 | 3/M | PRCA, neutropenia | MSD BM | Bu/cy | MMF/CsA | Colon grade 3-4 | No | VZV | ITP | 3 y >95% | 76 |
| P009* | 2016 | 5/M | Recurrent TIA, immunodeficiency | 10/10 MUD PB (2 boosts for declining chimerism) | Flu/treo/alem | MMF/CsA | Skin grade 1 | No | Adeno/HSV1/BK | PRCA, neutropenia | 1 y >95% | 15 |
| P010 | 2016 | 23/M | Severe lymphopenia, hypogammaglobulinemia | 10/10 MUD BM | Flu/bu/alem | MTX/CsA | No | No | None | None | 6 mo >95% | 11 |
| P011 | 2016 | 5/F | PRCA, neutropenia | 10/10 MUD BM | Flu/treo/TT/alem | MMF/CsA | Skin grade 1 | No | CMV, EBV | None | 6 mo 100% | 10 |
| P012 | 2014 | 23/F | Severe neutropenia | 10/10 MUD BM | Flu/mel/alem (RIC) | Prednisone/CsA | No | No | None | None | 2 y 98% | 39 |
| P013 | 2015 | 7/M | PRCA | 10/10 MUD BM | Bu/cy/ATG | MTX/CsA | No | No | None | None | 1 y 100% | 21 |
| P014 | 2007 | 9/M | PRCA | MMUD PB (first HSCT from affected MSD) | Flu/TBI450/alem (RIC) | MTX/CsA | Skin grade 2 | Skin + liver moderate | CMV/adeno/BK | AIHA | 3 y 95% | 117 |
Adeno, adenovirus; aGVHD, acute GVHD; AIHA, autoimmune hemolytic anemia; alem, alemtuzumab; BK, BK polyomavirus; BM, bone marrow; bu, busulfan; cGVHD, chronic GVHD; CMV, cytomegalovirus; comp, complications; cy, cyclophosphamide; EBV, Epstein Barr virus; flu, fludarabine; GF, graft failure; haplo, haploidentical; HHV, human herpesvirus; mel, melphalan; MMUD, mismatched unrelated donor; MSD, matched sibling donor; MTX, methotrexate; MUD, matched unrelated donor; PB, peripheral blood; RIC, reduced intensity conditioning; tacro, tacrolimus; treo, treosulfan; TT, thiotepa; VZV, varicella zoster virus.
Siblings.
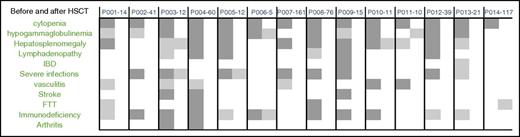
All patients engrafted at a median of day +20 for neutrophils and at day +23 for platelets. All patients are alive and well with a median follow-up of 18 months (range, 5 months-13 years). All patients had resolution of the hematological and immunological phenotype and no further vascular events were reported in 13/14 patients (Figure 1). One patient suffered from a pineal gland hemorrhage immediately post-HSCT at the time of prolonged thrombocytopenia as described previously.18 He has had no further vascular events since with a follow-up of 76 months. Chimerism analysis showed full donor white blood cell chimerism in all patients. ADA2 plasma enzyme activity normalized in all patients in whom ADA2 activity was monitored post-HSCT (n = 7) (Table 2). This occurred as early as 14 days post-HSCT, concurring with monocyte reappearance in the peripheral blood as verified by prospective monitoring of plasma ADA2 enzyme activity in 1 patient (I.M., unpublished observation). As for HSCT-related morbidity, 2 patients developed veno-occlusive disease, which responded to fluid restriction. Acute GVHD developed in 6/14 patients and resolved after standard treatment. Moderate chronic GVHD developed in only 1 patient. Viral reactivation was a frequent complication post-HSCT, occurring in 10/14 patients. Adenoviremia was the most common in 6/14 patients (42%). The patients who developed more than 2 viral reactivations all received peripheral blood stem cells. Post-HSCT hematological autoimmune phenomena were reported in 4 of 14 patients: ITP in 2, AIHA in 1, and neutropenia with immune-mediated PRCA in 1, responding to various treatment regimens (high-dose intravenous immunoglobulin/steroids/sirolimus/rituximab/bortezomib/romiplostim). Alopecia as a feature of DADA2 was present in 1 patient and completely resolved post-HSCT.
Effect of HSCT in clinical features resolution. Dark gray squares represent the presence of a clinical feature/phenotype. Light gray squares represent major improvement in clinical features. White squares represent complete resolution of clinical feature. Each patient is presented by 2 attached columns (before and after transplant) for comparison. Follow-up time post-HSCT for each patient is shown in months (first row). Severe infections represent any viral, bacterial, or fungal infection that required antiviral or antifungal treatment or led to sepsis. FTT, failure to thrive.
Effect of HSCT in clinical features resolution. Dark gray squares represent the presence of a clinical feature/phenotype. Light gray squares represent major improvement in clinical features. White squares represent complete resolution of clinical feature. Each patient is presented by 2 attached columns (before and after transplant) for comparison. Follow-up time post-HSCT for each patient is shown in months (first row). Severe infections represent any viral, bacterial, or fungal infection that required antiviral or antifungal treatment or led to sepsis. FTT, failure to thrive.
Discussion
We report the results of the first international survey on the outcome of HSCT for DADA2. The results support the use of HSCT as a definitive cure for DADA2, with 14 of 14 patients alive and well and 12/14 patients off all treatment at a median time post-HSCT of 18 months. Two patients are still on immunosuppression because they are less than 1 year out of HSCT. HSCT proved curative for the hematological, immunological, and vascular phenotype associated with the condition. Although the number of patients reported here is too limited to issue a general recommendation for HSCT in DADA2, the data clearly support the feasibility of HSCT as a definitive treatment option.
Importantly for all the DADA2 patients described here, the indication for HSCT was the hematological and/or immunological disorder, whereas the disease emphasis in the initial reports was on the vasculopathy with livedo, polyarteritis, and lacunar infarction. Indeed, PRCA, severe neutropenia, and refractory thrombocytopenia as well as combined immunodeficiency (including recurrent infection with Herpesviridae) prevailed in all transplanted patients. Before HSCT, treatment with tumor necrosis factor inhibitors (etanercept, infliximab) was attempted, but proved unsuccessful in 4 patients, and interleukin-1 receptor antagonist (anakinra) failed in 2 patients as far as restoration of the hematological and immunological phenotype was concerned. HSCT not only resolved the hematological and immunological phenotype, it also resulted in resolution of the vascular phenotype in all 6 patients who had vasculitis before HSCT. Only 1 patient experienced a single vascular event early post-HSCT at the time of severe thrombocytopenia. The same patient had an episode of late veno-occlusive disease, which responded to fluid restriction. No further vascular events were reported in any of the transplanted patients, in line with the current notion that the basic pathophysiology lies in macrophage skewing toward an M1 proinflammatory phenotype and that the vasculopathy phenotype can also be cured by HSCT. In this limited number of patients, no genotype-phenotype correlation could be found. Therefore, the mere presence of a given mutation alone cannot support the decision to proceed to HSCT for this rare condition; rather, the phenotype should be weighed in the decision to proceed to HSCT or to provide conventional treatment.
As is clear from our data, donor selection is important. Before the genetics of the disease were unraveled, 2 patients received a graft from apparently healthy sibling donors who later were shown to carry disease-causing CECR1 mutations and to be ADA2 deficient, resulting in engraftment failure. The question of whether a sibling donor who carries a single deleterious mutation in CECR1 is a good option remains unclear at present. However, it can be considered safer to opt for a matched unrelated donor in these cases given that a drop in chimerism in 1 patient resulted in PRCA. Moreover, at present, because absent ADA2 activity has been reported in patients with monoallelic CECR1 mutations, haploinsufficiency of CECR1 cannot be excluded as a cause for minor disease manifestations. Because recipient cells may have impaired ability to reject graft hematopoietic cells, and because in cases of immunodeficiency, donor lymphocytes could have survival advantage over ADA2-deficient recipient cells, nonmyeloablative conditioning can be a reasonable option as shown in some of the reported patients. In addition, a reduced intensity conditioning regimen may be a reasonable option until there is a better understanding of what degree of donor chimerism is necessary to cure the disease.
Infectious viral complications were frequent in our cohort, although they did not result in mortality. Adenovirus reactivation was the most common viral complication, present in 6/14 patients (42%); this agrees with previously published reports.22,23 Thus, frequent prospective monitoring of patients and preemptive treatment is essential.
Importantly, post-HSCT hematologic autoimmune complications were common in our cohort (ITP, PRCA, AIHA, neutropenia), seen in 4/14 patients (28%). Previous reports suggested the association of post-HSCT autoimmune hematologic disorders with nonmalignant disorders, unrelated donors, serotherapy, and younger age at HSCT.24-26 In our cohort, the association with serotherapy, in particular alemtuzumab, and younger age at HSCT might represent a potential explanation. However, at present we have no solid explanation for the autoimmune phenomena post-HSCT.
In conclusion, we report the successful treatment by HSCT in 14 DADA2 patients. All patients are alive and well and cured of immunological, hematological, and vascular manifestations. Thus, HSCT is an effective treatment option for definitive treatment of DADA2. Given the important morbidity and potential mortality associated with this disease, HSCT can be envisaged in any patient with DADA2 and severe immunological or hematological manifestations or even vasculopathy unresponsive to anti-inflammatory treatment. A matched unrelated donor can be considered in cases in which there is no unaffected matched sibling donor.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the affected children and their parents for their participation and for their confidence; the DADA2 Foundation (www.dada2.org) for its efforts in organizing the Inaugural International Conference on the Deficiency of ADA2; Chip Chambers for forming the foundation; Troy Torgerson and Daniel Kastner for facilitating and for advising on the data collection; Polina Stepensky for sharing invaluable information on patients with PRCA and DADA2; and Nancy J. Ganson and Susan J. Kelly, at Duke University Center, Durham, NC, for the numerous ADA2 enzyme activity measurements.
This paper was made possible thanks to the collaboration of the European Society of Blood and Bone Marrow Transplantation, Inborn Errors Working Party, Clinical Immunology Society, Primary Immunodeficiency Transplant Consortium, and the Center for International Blood and Marrow Transplant Research.
Authorship
Contribution: H.H. and I. Meyts collected, analyzed, and interpreted data, and wrote the manuscript; H.H., A.R.K., I. Müller, F.B., R.B., J.D., A.P.H., S.M.H., D.D.H., S.J., R.K., G.S., M.T., M.K., J.S., J.v.M., K.W., M.H., B.B., L.M., and I. Meyts provided clinical information from patients and edited the manuscript; M.H. provided the ADA2 enzyme assay activity for most of the patients and edited the manuscript; and all authors approved the final manuscript.
A complete list of the members of the Deficiency of Adenosine Deaminase Type 2 Foundation appears in “Appendix.”
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for H.H. is King Hussein Cancer Center, Amman, Jordan.
Correspondence: Hasan Hashem, King Hussein Cancer Center, P.O. Box 1269, Amman 11941, Jordan; e-mail: hasankamalhashem@yahoo.com; and Isabelle Meyts, University Hospitals Leuven, Department of Pediatrics, Herestraat 49, 3000 Leuven, Belgium; e-mail: isabelle.meyts@uzleuven.be.
Appendix: study group members
The members of the Deficiency of Adenosine Deaminase Type 2 Foundation are: Dan Kastner, Michael Hershfield, Troy Torgerson, Ann Reed, Ivona Aksentijevich, Marco Gattorno, Isabelle Meyts, Susa Benseler, Chip Chambers, Paul Brogan, Amanda Ombrello, Pnina Navon Elkan, and Yackov Berkun.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal