To the editor:
The prognosis of sickle cell anemia (SCA), initially disastrous in the severe forms of the disease, has greatly improved, leading to increased life expectancy. More than 95% to 99% of the children diagnosed with SCA in developed countries will become young adults, reaching reproductive age and able to consider having children of their own.1,2 Hydroxyurea (HU) is the main therapy that has considerably modified the prognosis of SCA,3,4 allowing, with good compliance, a substantial decrease in morbidity and mortality and significant improvement in quality of life.
Only 3 groups,5-7 including our own,5 have reported the potentially detrimental effect of HU on sperm parameters, when initiated in adult patients. These retrospective studies were performed among as few as 8 participants, without any comparative semen assessment before initiation of HU in 7 participants.5,7 On the basis of this observation, a prospective multicenter study was designed to assess the effect of 6 months of HU treatment (representing 2 complete cycles of spermatogenesis) on total sperm count (TSC; millions per ejaculate) in 35 men with severe forms of SCA.
All patients were volunteers and provided written informed consent. The trial was approved by the Committee for the Protection of Human Subjects in Biomedical Research (CPP Ile-de-France IV). The HYDREP (Hydroxyurea and Reproduction) study is registered in the European Clinical Trials Database as EudraCT (EUD-2009-017940-15) and at www.clinicaltrials.gov as #NCT01609192.
Patients eligible for a first treatment with HU8 were recruited by 2 sickle cell referral centers and 1 internal medicine department. They were between 18 and 60 years of age, and all were sexually active. Exclusion criteria were previous history of gonadotoxic treatment or any situation having an impact on spermatogenesis. HU was prescribed orally, at a dose of 15 to 30 mg/kg body weight per day, according to monitoring of hematological tolerance. Compliance with HU treatment was assessed by questioning and analysis of hematological impregnation (decrease in white blood cells, increase in mean corpuscular volume, and hemoglobin and fetal hemoglobin levels). Taking into account these criteria, all participants seemed adherent to HU therapy.
Men with SCA were then referred to members of the French national sperm-banking network Centre d’Etudes et de Conservation des Œufs et du Sperme Humains at Tenon, Cochin, or Jean Verdier Hospital. Their medical histories were recorded and sperm parameters analyzed according to World Health Organization 2010 guidelines.9
The TSC was obtained by multiplying the number of spermatozoa per milliliter by the volume of ejaculate. Normal values for volume and TSC are ≥1.5 mL and ≥39 million sperm per ejaculate. Patients with no sperm cells, after centrifugation of their ejaculate, were defined as azoospermic, and those with rare sperm cells were defined as cryptozoospermic. In the latter case, TSC was defined as 0.001 million sperm per ejaculate to simplify the statistical analysis. The rest of the semen was cryopreserved, according to the patients’ decision. Six months after the beginning of HU, another sperm sample (M6) was collected, analyzed, and compared with initial results (M0).
For statistical analysis, the sample size needed was calculated using the hypothesis of a 5-time reduction in spermatozoa concentration,5 which meant that at least 34 patients were required (two-tailed α = 0.05 and β = 0.2). The study population comprised 35 patients, an appropriate number for the required statistical significance.
Categorical variables were compared using the McNemar test, and quantitative variables were compared using the paired Student t test or nonparametric Wilcoxon rank sum test. All tests were two sided, and P < .05 was considered statistically significant. Statistical analyses were performed with SAS software (version 9.3; SAS Institute, Cary, NC).
Mean (± standard deviation [SD]) age of the 35 patients was 33.6 ± 9.2 years (range, 20-51 years), mean weight was 66.3 ± 8.9 kg (range, 53-92 kg), and mean height was 177.5 ± 8.3 cm (range, 151-194 cm). Mean (± SD) body mass index was 21.1 ± 2.7 kg/m2 (range, 16.4-28.1 kg/m2). Mean (± SD) age at beginning of puberty was 16.2 ± 2 years (range, 12-21 years). No overconsumption of alcohol, tobacco, or drugs was noted.
Before introduction of HU treatment (M0), 40% of the patients (14 of 35) had an abnormal TSC value; a single cryptozoospermia was seen but no azoospermia. This baseline finding confirmed the alteration of sperm parameters related to the SCA itself and has already been reported.5,10-14
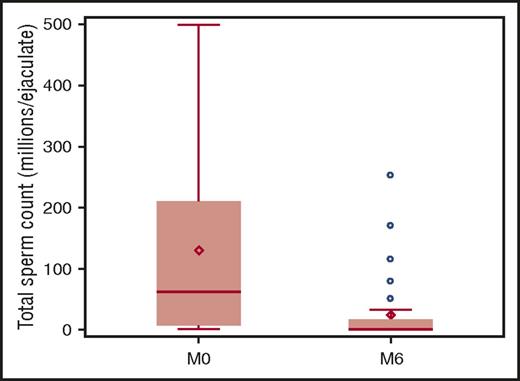
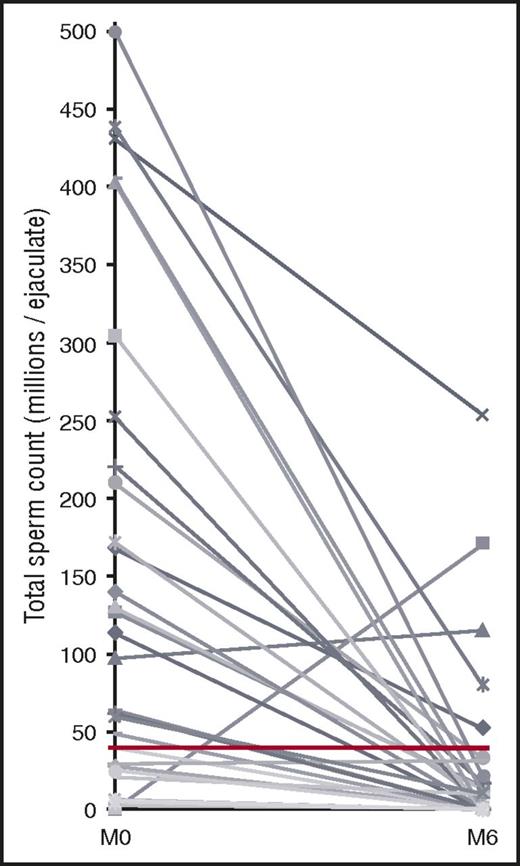
After 6 months of HU (M6), the mean (± SD) TSC decreased from 129.8 ± 150 million at M0 to 24.1 ± 54.1 million at M6; the median was 61.6 million (range, 6.5-210 million) at M0 and 0.63 million (range, 0.0001-17 million) at M6 (P < .0001), representing a strong reduction by a factor of ∼5 (Figure 1). Just more than twice as many patients (30 of 35 vs 14 of 35) had an abnormal TSC value at M6 compared with M0 (86% vs 40%; P < .0001), and 86% (30 of 35) showed a decrease in their TSC at M6, whether normal or not at M0. Moreover, the number of cryptozoospermic (n = 5) and azoospermic participants (n = 6) increased more than 10-fold, reaching almost 1 in 3 patients (11 [31%] of 35 at M6 vs 1 [2.8%] of 35 at M0) and making natural conception almost impossible for them. Furthermore, among the 24 remaining patients, 19 were oligozoospermic at M6, and only 5 (14%) displayed a normal TSC, compared with 21 men at M0 (60%). The TSC profile at M0 and M6 for each patient is shown in Figure 2. HU treatment over 6 months had no impact on the semen volume, the other parameter involved in the determination of TSC (mean ± SD: 2.34 ± 1.66 mL at M0 vs 2.50 ± 1.97 mL at M6; P > .05).
Boxplot of TSC at inclusion (M0) and after 6 months of HU treatment (M6).
Profile at M0 and M6 of TSC for each patient. The red line corresponds to the normal TSC according to the World Health Organization (≥39 million per ejaculate).
Profile at M0 and M6 of TSC for each patient. The red line corresponds to the normal TSC according to the World Health Organization (≥39 million per ejaculate).
TSC at M6 was not significantly different according to blood transfusion status (mean TSC ± SD: 37.65 ± 82.86 million for patients receiving transfusions vs 19.34 ± 41.07 million otherwise; P = .64) or to clinical events such as history of priapism (mean TSC ± SD: 24.84 ± 50.16 million for the 26 patients with priapism vs 26.05 ± 60.82 million otherwise; P = .95) or painful vaso-occlusive crises occurring during the study (mean TSC ± SD: 21.76 ± 2.62 million for those with vaso-occlusive crises vs 25.97 ± 7.36 million otherwise; P = .23). In addition, no correlation could be demonstrated between TSC at M6 and the prescribed individual HU dose (milligrams per kilogram per day; ρ = −16%; P = .38). Finally, patient age had no influence on the TSC at M0 (ρ = 17%; P = .33) or M6 (ρ = 0.9%; P = .96).
Three questions remain to be answered that were not in the framework of our study on adult SCA men receiving HU for the first time, a treatment usually pursued for years. Whether the reduction in TSC is reversible after cessation of HU remains 1 of these uncertainties. Indeed, other adverse effects of HU, such as blood count toxicity, do recover a few weeks after cessation of HU treatment, and a similar evolution could be hypothesized for the observed alteration in TSC. In the literature, only 5 patients with SCA had semen analysis before and after stopping HU therapy.5,6 Four men had altered sperm production, 1 of them remaining azoospermic four years after the cessation of any treatment. Thus, there are few data evaluating the reversibility of the adverse effects of HU on spermatogenesis, and long-term studies are required involving an adequate cohort of participants for proper counseling of our patients.
Another major unknown factor concerns the effect of HU treatment on spermatogenesis when initiated in children with SCA. In a unique report involving 4 patients, who were still receiving HU treatment at the time of the study, 2 experienced severe oligozoospermia and 2 experienced azoospermia after 8 and 15 years of treatment, respectively.15,16
The last unanswered question is related to the impact of HU on male fertility. Indeed, semen analysis is not a test of fertility, and even patients with severe abnormalities may father children. Our study, limited to a 6-month period, was not designed to clarify this point.
In summary, this comparative prospective study allows us, for the first time, to clearly answer the question of whether HU therapy has a potentially detrimental effect on spermatogenesis in patients with SCA: HU, at current doses, causes significant, rapid, and unpredictable impairment of spermatogenesis in treated men. These results may lead to consideration of preventive sperm cryostorage for adult patients with SCA requiring this treatment.17,18 This option was well accepted in our study; all included patients wanted to cryopreserve their sperm before HU treatment. Moreover, sperm banking helped to optimize HU adherence by reassuring those patients worrying about the potential impact of the treatment on their spermatogenesis.
Authorship
Acknowledgments: The HYDREP study was supported by a grant from the French Ministry of Health (Programme Hospitalier de Recherche Clinique 2009). The authors acknowledge the Centre de Ressources Biologiques GERMETHEQUE, the biobank in which the samples were stored before DNA fragmentation assays. The authors are indebted to Nadine Proust, Danielle Cesari, and Charlotte Gresle for their excellent technical assistance in semen analysis and to Françoise Shenfield for her relevant help with the English of the manuscript. The authors also thank the clinical research assistant team of Unité de Recherche Clinique de l’Est Parisien (University Paris 06, APHP) for trial monitoring and handling, preparation, and submission of all required research ethics and regulatory documents. Additional investigators: Robert Girot, Service d’Hématologie, Hôpital Tenon, University Paris 06, APHP, Paris, France; Pablo Bartolucci, Justine Gellen-Dautremer, Ruben Nzouakou, Ketty Lee, and Christine Fauroux, Service de Médecine Interne, Hôpital Henri Mondor, University Paris 12, APHP, Créteil, France; Vanina de Larouziere and Rachel Lévy, Service de Biologie de la Reproduction, CECOS, Hôpital Tenon, University Paris 06, APHP, Paris, France; Jean-Marie Kuntsmann, Service de Biologie de la Reproduction, CECOS, Hôpital Cochin, University Paris 05, APHP, Paris, France; and Jérôme Stirnemann, Service de Médecine Interne, Hôpital Jean Verdier, University Paris 13, APHP, Bondy, France.
Contribution: J.M. was the principal investigator and takes primary responsibility for the paper; D.B., K.S., A.H., L.L.-D., F.G., and F.L. recruited the patients; I.B., C.C., F.E., and C.R. performed the laboratory work for this study; S.B.-T. performed the hormonal assays; S.K. and T.S. did the statistical analysis; A.B. provided assistance with iconography; I.B. and J.M. coordinated the research and wrote the paper; and all authors participated in study conception and critical revision of the manuscript for intellectual content.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Isabelle Berthaut, Service de Biologie de la Reproduction, CECOS, Hôpital Tenon-4, Rue de la Chine, 75020 Paris, France; e-mail: isabelle.berthaut@aphp.fr.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal