In this issue of Blood, Guglielmelli et al highlight the importance of distinguishing prefibrotic/early primary myelofibrosis (pre-PMF) from overt primary myelofibrosis (overt-PMF) as a separate prodromal subgroup of myeloproliferative neoplasm (MPN).1 Before the World Health Organization (WHO) 2016 classification, pre-PMF was neither generally accepted in the scientific community as a distinct subgroup of MPN nor aligned with overt-PMF.2 In this study, the authors provide evidence that pre-PMF represents a prodromal stage of overt-PMF, and that it is clearly different from essential thrombocythemia (ET). With respect to clinical, hematologic, and molecular phenotypes, pre-PMF is associated with better risk factors that result in prolonged overall survival, as well as leukemia-free and fibrosis-free survival, when compared with overt-PMF. However, as has been reported in earlier studies, pre-PMF showed a significantly shorter overall survival than ET.3-5 Patients with pre-PMF are younger compared with patients with overt-PMF. Patients with overt-PMF have greater hematologic abnormalities (anemia, leukopenia, thrombocytopenia, higher blast counts), are more symptomatic, have larger spleens, and have a higher frequency of high molecular risk mutation profiles. Interestingly, the cohort of patients with pre-PMF had a predominance of female patients, which suggests the possibility that male patients progress to overt-PMF faster as the sex distribution is balanced in the later cohort.
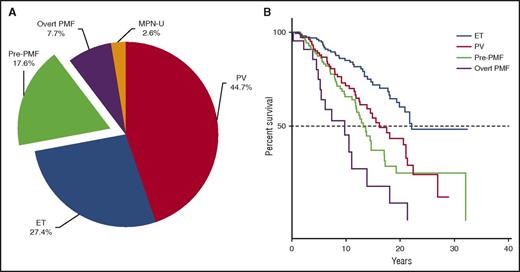
(A) Prevalence and (B) observed survival of pre-PMF as a distinct entity from other MPN (N = 807). Data from the Austrian Reclassification Project.10 MPN-U, myeloproliferative neoplasm unclassified; PV, polycythemia vera.
(A) Prevalence and (B) observed survival of pre-PMF as a distinct entity from other MPN (N = 807). Data from the Austrian Reclassification Project.10 MPN-U, myeloproliferative neoplasm unclassified; PV, polycythemia vera.
Since the late 1990s, a number of clinicopathological studies including follow-up examinations with repeated bone marrow (BM) biopsy evaluations have validated the existence of a precursor stage of overt-PMF (reviewed by Barosi,6 this finding was not recognized in classification systems).5,7 The results of the present paper are very supportive of pre-PMF being its own sub-entity among MPN, but should stimulate further clinical research and will, certainly, change routine procedures in clinical practice. First of all, this investigation confirms that it is mandatory to perform a BM biopsy in all patients newly diagnosed with MPN to estimate survival and optimize treatment decisions.3,5,8 Second, the present investigation demonstrates that spleen size and grade of BM fibrosis, as well as lactate dehydrogenase level, hitherto underreported, may display the severity of the disease.9 Third, when the International Prognostic Scoring System (IPSS) is applied in pre-PMF, the striking difference in clinical phenotypes between pre-PMF and overt-PMF influences the predictive value of this score with a superimposable median survival of more than 10 years for patients scored as intermediate 1 or intermediate 2. The IPSS, important for decision making for allogeneic stem cell transplantation in overt-PM, may therefore not be an adequate tool for such decisions in pre-PMF. Finally, and most importantly, the authors show that a high molecular risk profile is associated with a shorter survival not only in overt-PMF but also, when present, in pre-PMF. This is a new finding and will certainly change clinical procedures.
This study in a multicenter, real-life scenario demonstrated that the WHO 2016 classification is reproducible, with the caveat that the assignment to the different subgroups of MPN was not centrally reviewed by experienced hematopathologists. This study should stimulate similar analyses with descriptions of clinical and molecular differences between ET and pre-PMF, as this distinction is becoming more and more important for treatment decision making with the development of new treatment options for MPN. Finally, the prevalence of an MPN subgroup of pre-PMF comprises 15% to 25% of all patients with MPN; however, the exact numbers can only be determined by evaluations in centers with a diagnostic mandatory BM biopsy examination at entry of the patients (see figure).10 The overall survival of this patient group is comparable to that of patients with PV. With this new landmark analysis, it is clear that pre-PMF cannot be ignored as a separate subgroup of MPN. It requires management strategies that are different to those of ET and of overt-PMF. As suggested by the authors, prospective clinicopathological studies should be launched, including centralized evaluation of diagnostic BM biopsy slides, not only to establish the prevalence of pre-PMF and to confirm morphological features but also to further confirm the reproducibility of the WHO-defined criteria of pre-PMF.
Conflict-of-interest disclosure: H.G. receives research funding from Novartis and AOP Orphan, as well as speakers honoraria from Novartis, AOP Orphan, and Shire.