Abstract
*AR and AN contributed equally to the abstract
Background: When considering a high risk, but potentially curative procedure, such as an allogeneic hematopoietic stem cell transplantation (HSCT), prognostic models may help decision making. We have previously developed the Acute Leukemia (AL)-EBMT score for prediction of mortality following allogeneic HSCT in AL patients (Shouval et al., JCO, 2015). The score is based on 10 variables including: disease status,Karnofsky performance status, recipient age, diagnosis, interval between diagnosis to HSCT, conditioning regimen, donor type, donor and recipient CMVserostatus combination, HSCT year, and center experience (HSCT/year). External validation of the score on an independent cohort of AL patients is of importance.
Methods: This was a retrospective validation study on an independent cohort of AL patients from the Italian national transplantation network (GITMO). Inclusion criteria included adult AL patients, receiving an allogeneic HSCTbetween 2000-2014. Competing risks analysis was used to calculate the 2 years non-relapse related mortality (NRM) cumulative incidence, using the Gray test to test differences between ADT score groups. Overall survival (OS), and leukemia free survival (LFS) at 2 years were estimated using the Kaplan-Meier method; hazard ratios were computed between subgroups using Cox regression for OS and LFS and competing risk regression for NRM. Competing risk regression was used to compute NRM cumulative incidence rates, considering non-transplant mortality as the competing event. The predictive ability of the AL-EBMT score was assessed using time-dependent receiver-operator curves (AUC) analysis.
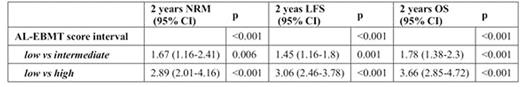
Results: A total of 1,848 patients from 61 Italian transplant centers were analyzed. The median age was 45.9 (IQR 35.2-55). Indications for HSCT were Acute Myeloid Leukemia (67.8%) and Acute Lymphoblastic Leukemia (32.2%). The majority of patients were in first complete remission (60.6%), and received myeloablative conditioning (81.3%). Median follow-up was 2 years (1.9-2.1, 95% CI). The AL-EBMT score was categorized according totertiles (low, intermediate, high) on the original ALWP-EBMT cohort. Increasing score intervals corresponded with decreasing probability for 2 year OS (95% CI), ranging from 75.52% (70.69-80.68) to 36.93% (32.81-41.56), and increasing probability of 2 years NRM ranging from 10.9% (7.97-14.93) to 27.39% (23.84-31.48) (Table 1, Figure 1). The highest scoring group was associated with a hazard ratio (95% CI) of 2.89 (2.01-4.16) for 2 year NRM and 3.66 (2,85-4.72) for death at 2 years (Table 2). The categorized score discrimination (AUC) for 2 year OS, LFS, and NRM was 66.42, 66.15, and 67, respectively.
Conclusion: This is the first study externally validating the AL-EBMT score. The score identified 3 distinctive risk groups and was predictive of survival related outcome. It can be used as a decision support tool when considering an allogeneic HSCT in acute leukemia patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal