Abstract
Background
The shared knowledge regarding management and outcome of PCNSL patients are usually based on results of clinical phase II studies that include limited series of selected patients, which imperfectly reflect the medical care in "real life".
Methods
The LOC network, certified by the national cancer institute (INCa), is a national network of expert centres for PCNSL. Since 2011, we are prospectively recording in the LOC database all newly diagnosed PCNSL patients from the 22 regional expert centres for PCNSL that cover the whole country. Data from PCNSL patients registered in the LOC database from January 2011 to March 18, 2016 were analyzed.
Results
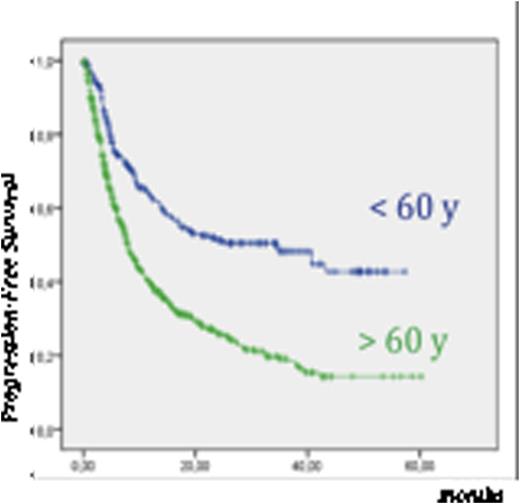
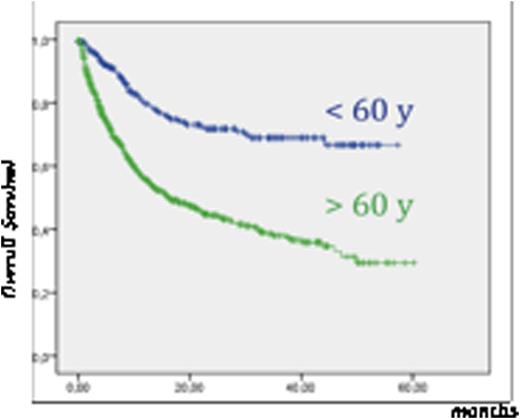
Data from 971 patients were available in the LOC database at the time of analysis: sex ratio: 1.05, median age: 67 (18-92), median Karnofsky Performance Status: 60 (20-100), diffuse large B cell lymphoma: 97%, ocular involvement: 20%, cerebrospinal (CSF) involvement: 18%. Diagnosis procedure was biopsy (80%), tumor resection (9%), vitrectomy (8%), CSF cytology (3%). Treatment was initiated either by a neuro-oncology or a haematology team in 38% and 62%, respectively. Median delay between first symptoms and onset of treatment was 62 days. First line treatment was high-dose (HD) methotrexate (MTX) based chemotherapy (CT) (90%), other chemotherapy regimen (6%), or palliative care (4%). The use of Rituximab has gradually increased from 50 % of patients between 2011 and 2013, up to 87 % of patients in 2016. 16 % of patients were included in prospective trials. After first-line induction chemotherapy, responder patients < 60 years received a consolidation treatment in 75 % of cases consisting of either whole brain radiotherapy (WBRT) (49 %) or HD CT with autologous stem cell transplantation (HD CT-ASCT) (26 %). Low dose WBRT (23,4) is being used in younger CR patients since 2014. In responder patients > 60 years, WBRT was seldom given (9%) according to national guideline, and HD CT-ASCT was offered to 1% of patients. Response rates to first-line treatment among evaluable patients (n = 655) were: complete response: 59%; partial response: 10%; stable disease: 3%; progressive disease: 28%. Relapse occurred in 42 % patients < 60 y and in 62 % in older patients. At relapse, second line chemotherapy, HD CT-ASCT, WBRT and palliative care were offered in 50%, 18%, 12%, 20% of patients respectively. With a median follow-up of 20.4 months, median progression free survival (PFS) was 9.9 months for the whole population (< 60 years: 34.6 months; > 60 years: 7.9 months). Median overall survival (OS) and 5-year OS were 30 months and 41% respectively (< 60 years: not reached, 68%; > 60 years: 15 months, 30%).
Conclusion
The therapeutic practices in France reflect the current knowledge and controversies in PCNSL. Long-term survival has become frequent, especially among youngest patients who usually receive a consolidation treatment and to whom HD CT-ASCT can be offered at relapse. Relapse rate remains frequent and especially in elderly patients in whom consolidation treatment is omitted. Such an overview points out a couple of issues. Despite homogeneous treatments following national guidelines in accordance with the state of the art of medical care, standards of care are to be challenged, both for increasing the CR and decrease the relapse rates. The development of target and innovative therapies in PCNSL alone or in combinatorial regimen is needed.
PFS and OS of patients according to age
Soussain:Roche: Research Funding; Celgene: Research Funding; Pharmacyclics: Research Funding. Ghesquieres:Mundipharma: Consultancy; Roche France: Research Funding; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees. Choquet:Janssen: Consultancy; Celgene: Consultancy. Morschhauser:Servier: Consultancy, Honoraria; Janssen: Honoraria; Gilead Sciences: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Roche: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal