Abstract
Acute myeloid leukemia (AML) is a disease with a high incidence of relapse and mortality. Relapse is attributed to the inability of current chemotherapeutic agents to eliminate leukemia stem cells (LSCs). Thus, to improve leukemia therapy, it is critical to identify agents that effectively target LSCs, e.g. via unique cell surface antigens. A target of major interest is CD123, the transmembrane alpha chain of the interleukin-3 receptor, expressed on blasts, leukemic progenitor and LSCs in the majority of AML patients. We have developed an allogeneic chimeric antigen receptor (CAR) T-cell platform using T-cells from third-party healthy donors to generate engineered T-cells targeting CD123 (UCART123). UCART123 cells no longer express a TCR, having undergone a disruption of the TCRα gene using TALEN¨ gene editing technology followed by elimination of TCRα/β-positive cells, thus minimizing the potential for engineered T-cells to cause graft versus host disease (GvHD). We tested the activity of UCART123 cells in vitro using primary AML samples, normal bone marrow (nBM) and cord blood (CB) cells. Additionally, we established patient derived xenograft (PDX), nBM- or CB- humanized xenografts (HuX) and a competitive nBM/AML xenograft model to evaluate the in vivo potential of UCART123 cells to preferentially eliminate AML over normal BM cells.
In vitro studies reveled that UCART123 cells eliminate AML cells and had minimum effect on normal cells at effector:target ratios as low as 0.5:1. Next, we evaluated the in vivo activity of UCART123 against PDX (AML37, TP53 mutant relapsed AML and AML20, FLT3-ITD+ and TP53 mutant AML) and normal-HuX mice (n=3). At 3 weeks post T-cell injection we found that UCART123 treatment eliminated the leukemic cells when using 10M or 3M UCART123 cells per mouse and no significant difference between PBS or TCR-deficient T-cells (TCRkoT; 10M/mouse). Toxicity to normal cells was dose dependent, doses of 2.5M UCART123 cells did not significantly affect hematopoietic cells. T-cells were detected in the BM at day 14 after treatment, without evidence of GvHD.
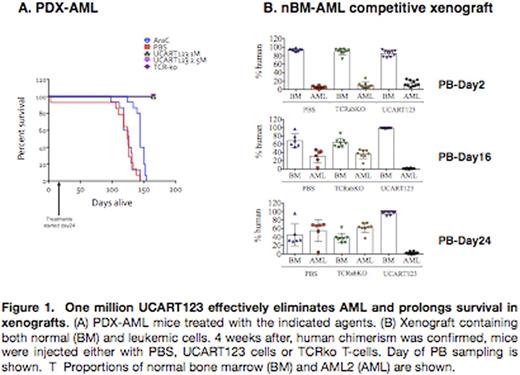
Since we found complete elimination of human AML cells in the BM of the PDX precluding serial transplantation to evaluate LSC activity, we initiated two new sets of PDX-AML mice [AML2 (NPM1+FLT3-ITD+) and AML37 (TP53 mutant)] to evaluate long-term survival, and time to relapse. Animals were treated with PBS, UCART123 (2.5M or 1M), TCRkoT (2.5M), or Ara-C (60mg/kg 5 days). Animal weight and peripheral blood (PB) was monitored. Cytokines changes were evaluated at day 2. We found that the cytokine release and the kinetics of AML targeting by UCART123 were dose dependent. We found a significant overall survival (OS) benefit with UCART123 in both PDX tested. For example, all PDX-AML2 mice treated with UCART123 are alive to date (day 167; updates will be presented). All other cohorts were lost (PBS day124, TCRkoT day126, AraC day144) (Figure 1A).
Finally, to determine selectivity of UCART123 cells for AML cells over nBM cells, we generated a competitive model bearing both nBM and AML (NPM1+FLT3-ITD+). With PB monitoring, treatment with 1M UCAR123 cells resulted in selective elimination of AML cells. Untreated and TCRkoT treated mice showed a rapid progression of AML, while treated mice showed normal hematopoiesis (Figure 1B). NPM1 transcripts were also monitored in the mice and confirmed molecular remission in mice.
Taken together, our data show that UCART123, an "off-the-shelf" allogeneic engineered CAR-T product targeting CD123 potently eliminates AML cells in vivo, prevents relapse, and improves OS in PDX mice. Also, UCART123 cells preferentially targets AML cells in a competitive BM/AML model. A phase I trial of UCART123 in AML is under development.
Guzman:Cellectis: Research Funding. Sugita:Cellectis: Research Funding. Galetto:Cellectis SA: Employment. Gouble:Cellectis: Employment. Smith:Cellectis SA: Employment. Roboz:Agios, Amgen, Amphivena, Astex, AstraZeneca, Boehringer Ingelheim, Celator, Celgene, Genoptix, Janssen, Juno, MEI Pharma, MedImmune, Novartis, Onconova, Pfizer, Roche/Genentech, Sunesis, Teva: Consultancy; Cellectis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal