Abstract
Background: Chronic lymphocytic leukemia (CLL) is an indolent B-cell malignancy with approximately 18,960 patients expected to be newly diagnosed in 2016 in the United States. CLL is a heterogeneous disease and some patients can be managed with a 'watch-and-wait' strategy, but those with symptomatic or advanced disease may be candidates for active therapy. However, few studies have examined real-world treatment patterns, health care utilization, and costs. This study examined initial therapy received among CLL patients in the US, the associated health care utilization, and total healthcare costs, including patient out-of-pocket costs.
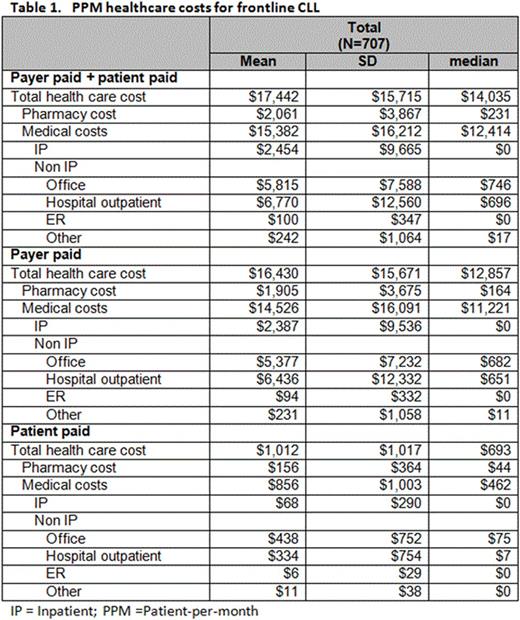
Methods: This retrospective studyused the Optum Research Database which includes medical and pharmacy claims from a large national US health plan to identify adults (≥18 years old) insured either commercially or through Medicare Advantage from 5/2013 - 6/2015, with ≥2 medical claims for CLL (ICD-9-CM code 204.1x). Pts required ≥1 claim for systemic cancer therapy; the first observed claim defined the index date. Continuous enrollment in the health plan for 6 months prior to index date (baseline period) and at least 1 month after index date (variable follow-up period) was also required. Pts with additional primary malignancies or who received systemic cancer therapy during the baseline period, and those who underwent stem cell transplant during the study period, were excluded. Therapeutic agents with a NCCN compendium listing for the treatment of CLL were assessed. Patient characteristics, initial regimen received, and duration of the first line of therapy were examined. Healthcare utilization and cost analyses for the entire cohort were descriptive in nature. Patient-per-month (PPM) counts of healthcare utilization and PPM costs were calculated. Costs included both health plan paid and patient out-of-pocket (OOP). Components of healthcare costs included inpatient (IP), non-IP medical, and drugs through the pharmacy benefit.
Results: There were 707 CLL pts who met all study criteria during the study period; 40% were commercially insured and 60% were Medicare Advantage enrollees. The most common regimens received as first line of therapy at the time of the analyses included Bendamustine and Rituximab (26%), Rituximab monotherapy (20%), Ibrutinib (14%), Fludarabine+Cyclophosphamide+Rituximab (FCR) (9%), Chlorambucil (7%), and Chlorambucil with Obinutuzumab (6%). The mean duration of first line therapy during the study period was 4.4 months (standard deviation [SD]=3.4). Among the study population, the mean baseline Charlson comorbidity index was 2.87 (SD=1.38) and most were male (65%). The mean age was 70 years (SD=11), but varied by regimen (overall p-value <0.01); the Chlorambucil cohort was the oldest (mean 80 years, SD=8) and the FCR cohort was the youngest (mean 60 years, SD=9). Overall, during first line of therapy, CLL patients visited physician offices and hospital outpatient facilities 3 and 2 times per month, respectively. In addition, 33% and 24% of patients had a least one ER visit or IP stay during the first line of therapy, respectively. The average total PPM healthcare costs for the entire cohort was $17,442 (SD=$15,715) (Table 1). Six percent of the average total PPM was patient OOP costs (mean $1,012). The majority of PPM costs were due to non-IP care (approximately 74% or $12,928), approximately 14% were due to IP care (mean $2,454), and 12% were due to pharmacy costs (mean $2,061).
Conclusion:
The majority of PPM costs among patients receiving frontline CLL treatment are attributable to visits in the outpatient and hospital outpatient settings followed by inpatient visits and pharmacy costs. Approximately 6% of the PPM healthcare costs are paid OOP by the patient. Total healthcare costs to the system and to the patient will depend on several factors, including adherence to drug regimens, time to progression, and whether regimens are prescribed for a fixed number of cycles or given until disease progression.
Dacosta Byfield:Optum: Employment; UnitedHealth Group: Equity Ownership. Blauer-Peterson:Optum: Employment; UnitedHealth Group: Equity Ownership. Montez:Genentech, Inc: Employment; Roche: Equity Ownership. Reyes:Roche: Equity Ownership; Genentech: Employment. Masaquel:Roche: Equity Ownership; Genentech, Inc: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal