Abstract
Introduction:
A significant source of morbidity and mortality related to allogeneic hematopoietic cell transplantation (HCT) is neurologic complication. We performed a retrospective chart review to determine the incidence, risk factors, timing, and impact of neurologic complications in the first five years after HCT.
Methods:
We performed a retrospective chart review of patients undergoing allogeneic HCT for hematological disorders at the Massachusetts General Hospital between January 2000 and December 2010, focusing on neurologic complications after HCT. We determined the incidence of central nervous system (CNS) infections, intracranial hemorrhage, thromboembolic events, metabolic encephalopathy, posterior reversal encephalopathy syndrome (PRES), seizures, CNS malignancy, and peripheral neuropathy. We classified neurological events as either early (day -7 to day +100), late (day +101 to 2 years) or very late (2 years to 5 years). Risk factors studied were demographics (age, gender, race), disease-related factors (diagnosis, disease status, prior autologous transplant),transplant factors (myeloablative or reduced-intensity conditioning, use of antithymocyte globulin (ATG), stem cell source and GVHD prophylaxis). Outcome variables were neutrophil and platelet engraftment, progression free survival (PFS) and overall survival (OS).
Results:
There were 263 consecutive patients (median age 54 years, range 18 to 76 years). The diseases were acute myeloid leukemia n=91 (34.6%), non-Hodgkin lymphoma n=64 (24.3%), myelodysplastic syndrome n=41 (15.6%), acute lymphoblastic leukemia n=21 (8.0%), myeloproliferative neoplasm n=13 (4.9%), chronic lymphocytic leukemia n=12 (4.6%), Hodgkin lymphoma n=11 (4.2%), multiple myeloma n=10 (3.8%). Conditioning was myeloablative n=86 (33%), or reduced-intensity n= 177 patients (67%). Donor source was matched related donor n=153 (58.1%), matched unrelated donor n=52 (19.8%), haploidentical n=35 (13.3%), umbilical cord blood n=20 (7.6%), and mismatched unrelated donor n=3 (1.1%). The median days to ANC > 500x106/L, and platelet count > 20,000 x106/L unsupported were 15 (range 7 to 37 days) and 19 (range 7 to 167 days), respectively. The incidence of acute GVHD grades II-IV was 22% and the 1-year incidence of extensive chronic GVHD was 8.9%. The 5-year overall and progression free survivals were 37% and 29% respectively. The major cause of death was relapsed or progressive malignancy.
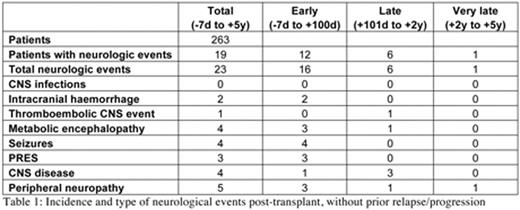
15 patients (5.7%) experienced 19 clinically active neurologic events without having relapsed or progressed at the time, as follows: CNS infection n=0,CNS hemorrhage n=2, CNS thromboembolic event n=1, metabolic encephalopathy n=4, PRES n=3, seizure n=4, CNS malignancy n=4, and peripheral neuropathy n=5 (Table 1). 4 patients experienced CNS relapse as their first neurologic event post transplant. Patients who relapsed or progressed had a higher incidence of neurologic complications -55 of those patients (38.4% of patients who relapsed) experienced 79 neurologic events: CNS infection n=16,CNS hemorrhage n=14, CNS thromboembolic event n=14, metabolic encephalopathy n=14, PRES n=3, seizure n=9, CNS disease n=7, and peripheral neuropathy n=12(Table 2). After 100 days post transplant, neurologic complications were rare in patients who had not relapsed or progressed (2.2% of patients). In a multivariate analysis, risk factors for neurologic complication were relapsed/progressive disease, grade II-IV acute GVHD and use of sirolimus in GVHD prophylaxis. 4 of 17 patients who received sirolimus had a neurologic event (1 thromboembolic stroke, 1 seizure/PRES, 1 seizure/PRES/metabolic encephalopathy and 1 peripheral neuropathy). Neutrophil and platelet engraftment were not affected by neurologic complications. Neurologic complications negatively impacted OS (Hazard Ratio (HR) 3.5, p<0.001) and PFS (HR 2.2, p<0.0001).
In summary, (1) Neurologic complications are uncommon after allogeneic HCT (5.7%); (2) Neurologic complications are more common in patients with relapsed or progressive disease (38.4%); (3) Neurologic complications are more common in patients receiving sirolimus-containing GVHD prophylaxis (23.5%), although limited by small numbers; (4) Neurologic complications are uncommon after 100 days (2.2%); (5) Neurologic complications were associated with decreased PFS and OS.
Chen:Novartis: Research Funding; Incyte Corporation: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal