Abstract
We are studying a novel mechanism by which prototypical erythrocyte proteins also act in endothelial cells to regulate vascular tone. Previously, we reported that the alpha subunit of hemoglobin (αHb) is expressed in the myoendothelial junction of endothelial cells in resistance arterioles where it binds endothelial nitric oxide (NO) synthase (eNOS) and degrades NO, thereby stimulating vasoconstriction. To extend this observation, we examined arterioles of mice lacking 2 out of 4 α globin genes [HbA1 knockout *α2/*α2]. Compared to wild type (wt) controls, the thoracodorsal artery (TDA, a resistance arteriole) from mutant animals exhibited abnormal morphology with thinned internal elastic lamina, excessive dilation, and reduced contractility after treatment with the vasoconstrictor phenylephrine (EC50 8.2e-6M-1 n=6 in wt vs 2.3e-5 M-1 n=6 in mutant; p<0.0001).
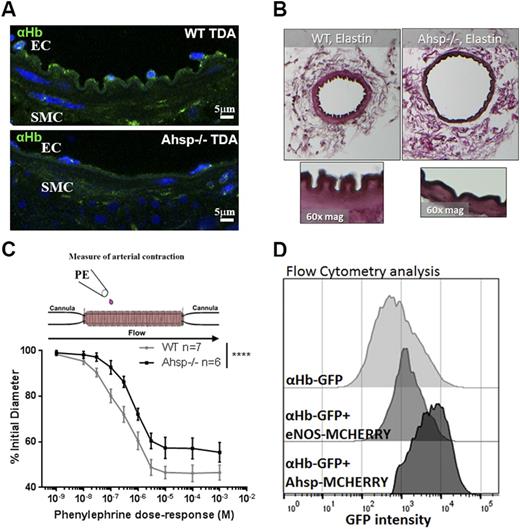
Wild type TDAs expressed αHb (Fig. 1A), but not βHb mRNA and protein. However, free αHb is unstable and not expected to exist as an isolated monomer. Alpha hemoglobin stabilizing protein (AHSP) is a molecular chaperone that binds free αHb, stabilizes its structure and facilitates assembly of HbA tetramers (α2β2) in red blood cells. Immunohistochemistry showed that AHSP and αHb co-localize in endothelial cells lining the TDA. In the TDA of Ahsp knockout (KO) mice, αHb immunostaining was disorganized and reduced in intensity (Fig. 1A), and Western blotting showed reduced αHb protein compared to wt controls. Moreover, TDAs from Ahsp KO mice exhibited abnormal thinning of the internal elastic lamina, excessive dilation (lumen diameter 7500 μM2 in Ahsp KO vs 4100 μM2 in controls; n=5 mice, p=0.0037) and reduced constriction after phenylephrine treatment (EC50 9.6e-6 M-1 in wt n=7 vs 5.6e-6 M-1 in mutant n=6; p<0.0001) (Fig. 1B-C), similar to what we observed in HbA1-/- mice.
To examine physical and functional interactions between AHSP, αHb and eNOS, we expressed fluorescent-tagged proteins in cultured human coronary ECs. αHb-GFP alone was expressed at relatively low level (mean fluorescent intensity (MFI) = 631) (Fig. 1D). Coexpressed mCherry-AHSP colocalized with αHb-GFP and increased its expression level (MFI 5312) (Fig. 1D). Similarly, coexpressed mCherry-eNOS colocalized with αHb-GFP and enhanced its expression (MFI 1519) (Fig. 1D). Purified αHb co-immunoprecipitated with AHSP or eNOS, but not both, suggesting mutually exclusive interactions.
Overall, our studies provide genetic evidence that αHb expressed in arteriolar endothelial cells regulates blood vessel tone in vivo. Moreover, biochemical studies show that AHSP stabilizes endothelial-expressed αHb and facilitates its assembly with eNOS. Thus, AHSP acts as a molecular chaperone for αHb in erythrocytes and endothelial cells to promote the formation of HbA (α2b2) for O2 transport, and αHb-eNOS for NO degradation. We hypothesize that the αHb-AHSP-eNOS axis functions to fine-tune systemic blood pressure and/or regional blood flow to specific vascular beds. Defining the magnitude of these effects in mice and humans during specific circulatory stresses and in α thalassemia is an important and interesting topic for future investigation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal