Abstract
Introduction: We previously reported the long-term efficacy and safety of pegylated interferon alpha-2a (PEG-IFN-a-2a) in 83 patients with ET and PV after a median follow-up of 83 months. Here, we present the bone marrow (BM) response assessment according to modified International Working Group for-Myeloproliferative Neoplasms Research and Treatment (IWG-MPN).
Objective: To identify histomorphological BM responses in patients with ET and PV treated with PEG-IFN-a-2a as part of a prospective phase II study.
Methods: All patients had BM assessment done prior to their enrollment, and then every 6-12 months while on study if possible, and in some patients after treatment discontinuation. Complete BM remission (BM-CR) required absence of > grade 1 reticulin fibrosis and disappearance of megakaryocyte hyperplasia in ET or trilinear hyperplasia with age-adjusted normocellularity in PV. An incomplete, partial response (BM-PR), was defined when fibrosis grading had consistently improved by at least one grade level on at least 2 consecutive samples > 12 months apart, yet with persistent MPN morphological features. Hematologic (HR) and molecular response (MR) assessments were previously reported (ASH 2015, abstract #60).
Results: Among 83 enrolled patients (43 PV, 40 ET), 58 patients (70%) had evaluable BM samples for histomorphological response assessment, with median number of 8 samples per patient (range, 3-12). Among the remaining 25 patients, 18 were treated ≤12 months, and 7 did not have representative samples. Median age was 52 years (range, 19-75), and 29% (n=17) were males. Median disease duration prior to enrollment was 31 months (range, 1-350), and the median exposure to PEG-IFN-a-2a was 80 months (range, 15-107). After a median follow-up of 84 months (range, 36-107), 32 patients are on study. Forty-two patients were JAK2 positive, 6 CALR positive, 2 MPL positive and 8 triple negative (TN). Hematologic and molecular (JAK2V617F mutation only) responses were seen in 54 (93%) and 29 (69% of JAK2V617F positive) patients, including complete HR and complete MR in 52 (90%) and 9 (31%) patients, respectively.
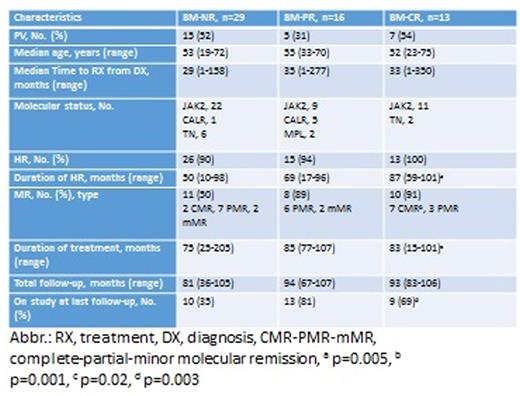
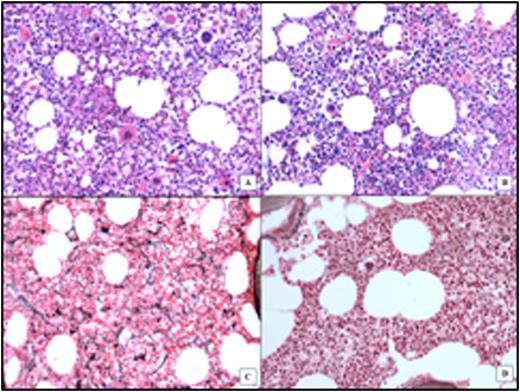
In total, 29 evaluable patients (50%) had BM response, including 13 patients (22%) with BM-CR (MF-0 in 11, example in Figure 1). Among 16 patients with BM-PR, 3 had resolution of dense collagen bundles as well as decreased reticulin fibrosis. Except for increased platelets in those with BM-PR (p<0.001), likely due to the higher proportion of ET patients in that group, no other differences in basic demographic or clinical parameters were present among different response groups (Table 1). Patients with BM response (PR & CR) had lower discontinuation rate, higher duration of response (HR & MR) with longer time on therapy; 13 patients with BM-CR had higher probability of complete MR (Table 1). Median time to BM-CR was 48 months (range, 30-72), median duration was 30 months (24-52), and has been maintained in 9 patients (69%). Two patients who lost their BM-CR are still on active therapy with persistent complete MR. Interestingly, 4 patients achieved BM-CR after being off therapy for a median of 18 months (range, 2-30), and 3 of them have sustained the BM-CR for 24, 50 and 52 months.
Conclusions: Histomorphological BM responses (including complete response) can occur in ET/PV patients treated with PEG-IFN-a-2a, and generally correlate with more durable treatment benefit. Complete BM responses may be sustained even after treatment discontinuation, or be seen after therapy discontinuation. Despite this, we could not identify a uniform correlation between hematologic, histomorphological and molecular response.
BM assessment of a PV patient with BM-CR. A & C: Before treatment: increased cellularity and abnormal megakaryocytes number/morphology; MF-2. B & D: After treatment: normocellular BM, normal morphology, MF-0.
BM assessment of a PV patient with BM-CR. A & C: Before treatment: increased cellularity and abnormal megakaryocytes number/morphology; MF-2. B & D: After treatment: normocellular BM, normal morphology, MF-0.
Cortes:ARIAD: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Teva: Research Funding. Konopleva:Reata Pharmaceuticals: Equity Ownership; Abbvie: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Stemline: Consultancy, Research Funding; Eli Lilly: Research Funding; Cellectis: Research Funding; Calithera: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal