Abstract
Introduction:
The advent of next generation sequencing (NGS) has brought intense interest to the complex genetic landscape of myeloproliferative neoplasms (MPN). However, data regarding clinical outcomes in the context of novel MPN therapies such as JAK inhibitors are scarce. Limited data indicate that high molecular risk signature (HMR, presence of at least one mutation in ASXL1, EZH2, IDH1/2, SRSF2) or multiple mutations may be associated with decreased spleen response and a shorter time to discontinuation of Ruxolitinib in myelofibrosis (Patel et al, Blood 2015).
Methods:
All myelofibrosis patients seen in the MPN program at Princess Margaret Hospital between November 2009 and May 2016 and treated with JAK1/2 inhibitor therapy were identified. NGS molecular profiling of 54 genes (39 hotspot region; 15 complete coding region coverage) was performed on peripheral blood or bone marrow samples using the TruSight Myeloid Sequencing Panel. Reporting was restricted to well-covered, exonic nonsynonymous, intronic splice site, and known pathogenic synonymous variants. Variants with global mean allele frequency >1% were identified using multiple population databases (1000 genomes, ESP, ExAC) and excluded. The primary endpoint was time from start of JAK1/2 inhibitor therapy to treatment failure (TTF) defined as treatment discontinuation, progression to accelerated phase or leukemic transformation, spleen progression or death. Secondary endpoints included best spleen, anemia and IWG response achieved by 48 weeks of treatment and overall survival. Response was assessed according to the 2013 revised IWG-MRT criteria. Transfusion dependency was assessed as any transfusion in 12 weeks prior to treatment or being identified as transfusion dependent in medical history.
Results:
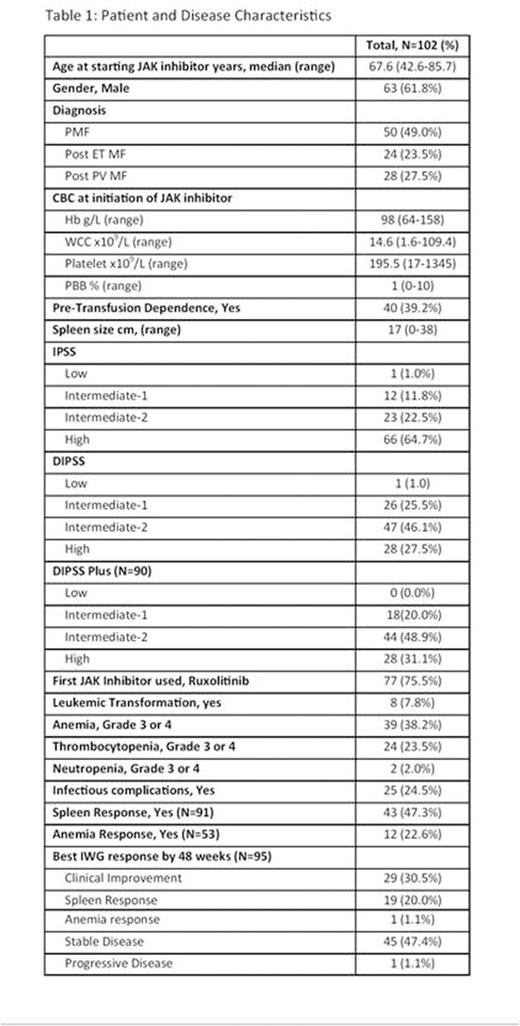
Of 159 patients treated with JAK1/2 inhibitors at our institution, 102 met the inclusion criteria (see Table 1). Patients were excluded if; no sample was available for analysis (19), short use of JAK inhibitor prior to transplant (9), active clinical trial (5), in accelerated phase/acute leukemia (4) and others (20). First JAK inhibitor used was ruxolitinib in 77 patients and momelotinib in 25. At least one mutation was identified in every patient. Twenty (20%) patients had one mutation, 32 (31%) had 2 mutations and 50 (49%) patients had ≥ 3 mutations. Eighty (82%) patients had the JAK2V617F mutation, 15 (15%) had mutations in CALR, 4 (4%) had MPL mutations and one patient was triple negative. One patient had mutations in both CALR and JAK2 while another had mutations in MPL and CALR. Forty-eight (47%) patients had mutations consistent with HMR profile. Mutation profile is summarized in Table 2.
With median follow-up of 2.5 years, 51 (50%) patients experienced treatment failure. On univariate analysis, TTF was associated with DIPSS, pre-treatment transfusion status and Hb <100 prior to initiating JAK inhibitor therapy. However, TTF was not associated with specific driver mutations, the number of mutations or HMR profile. Exploratory analysis of genes mutated in ≥5% of the population showed EZH2 (p=0.004) and CBL (p=0.005) mutated patients had shorter TTF. Multi-variable analysis employing anemia <100 and DIPSS with either of the number of mutations or HMR profile did not show any association with TTF. There was a trend towards TTF in patients with Hb<100 (HR 2.21, 95%CI: 0.99-4.95, p=0.05). Of 102 patients, 91 were evaluable for spleen response with 43 (47%) achieving a spleen response by 48 weeks of treatment. Twelve (23%) of the 53 patients evaluated met criteria for anemia response. Neither spleen nor anemia response was associated with the use of a particular JAK inhibitor. Of the 95 patients with at least 48-week follow-up, best response while on treatment was clinical improvement and spleen response in 29 (31%) and 19 (20%) patients respectively.
Conclusions:
In this study of myelofibrosis patients treated with JAK inhibitors, EZH2 and CBL mutated patients had shorter TTF. We did not find any association between TTF and number of mutations or other high risk mutations such as ASXL1/SRSF2. Anemia was the only significant independent predictor of shorter TTF. Our findings highlight the need for multicenter collaborative studies on a large number of patients and cautious use of mutation profiling results in routine clinical decision making with current treatment approaches.
Spiegel and McNamara are co-primary authors.
Panzarella:Cellgene: Consultancy. Schimmer:Novartis: Honoraria. Schuh:Amgen: Membership on an entity's Board of Directors or advisory committees. Yee:Novartis Canada: Membership on an entity's Board of Directors or advisory committees, Research Funding. Kamel-Reid:BMS: Research Funding. Gupta:Novartis: Consultancy, Honoraria, Research Funding; Incyte Corporation: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal