Abstract
Background: Pre-leukemic hematopoietic stem cells (HSC) have been implicated in AML (Jan et al STM 2012) and also for several lymphoid leukemias including ALL, HCL, and CLL. Separately, relapse of ALL following CD19 CAR-T cell therapy has been associated with lymphomyeloid lineage switch. Finally, healthy persons with clonally expanded HSCs are at increased risk of hematologic malignancies including lymphomas, and in mouse DLBCL models we previously demonstrated the oncogenic sufficiency of BCL6 overexpression in HSC (Green et al 2014 Nat Comm). Nevertheless, the cellular origin of DLBCL in the majority of patients is not definitively known. We sought to investigate the presence of mutations found in DLBCL within matched HSCs.
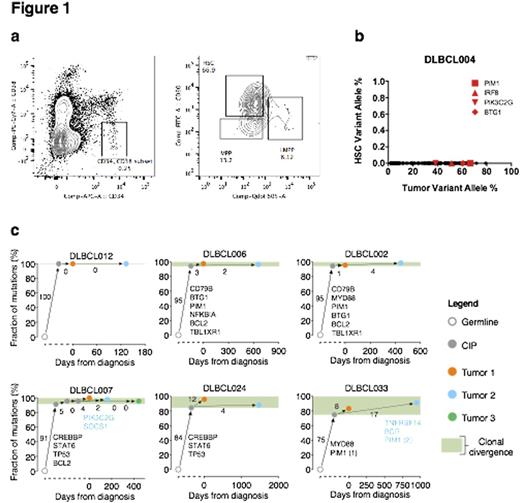
Methods: We deeply genotyped somatic mutations in diagnostic biopsy tissues of 16 patients with DLBCL using CAPP-Seq to a median sequencing depth of 1100x (Newman et al 2014 Nat Med; Scherer et al 2015 ASH). We then profiled each patient for evidence implicating HSCs using somatic mutation lineage tracing, in either direct or indirect fashion. For direct evaluation, we used highly purified, serially FACS-sorted HSCs from grossly uninvolved bone marrow (BM) (n=5; Fig 1a-b). For indirect assessment, we either profiled serial tumor biopsies (n=13), or interrogated sorted cells from terminally differentiated blood lineages (n=7), including peripheral CD3+ T cells, CD14+ Monocytes, and B cells expressing a light-chain discordant to that of tumor isotype. HSCs and differentiated lineages were then interrogated by direct genotyping, using 3 highly sensitive orthogonal quantitative methods, including Myd88 L265P droplet digital PCR (n=6), BCL6 translocation breakpoint qPCR (n=4), and DLBCL CAPP-Seq profiling of 268 genes (n=5). We used the theoretical limit of detection (LOD) genotyping performance for CAPP-Seq (0.001%, Newman et al 2016 Nat Biotech), and established analytical sensitivity of our custom MYD88 ddPCR via limiting dilution (~1%). These LODs met or exceeded the expected limit of sorting impurity by FACS (~1%). For 6 patients experiencing one or more DLBCL relapse, we deeply profiled 13 serial tumor biopsies by CAPP-Seq, and then assessed overlap in somatic mutations and VDJ sequences in biopsy pairs as additional indirect evidence implicating HSCs.
Results: We obtained a median of ~2000 sorted HSCs and ~1700 sorted cells from differentiated lineages, and genotyped each population using one or more of the 3 direct genotyping methods described above. Three patients with sufficient cell numbers were profiled both by CAPP-Seq and either ddPCR (n=2) or qPCR (n=1). Surprisingly, we found no evidence implicating HSCs either directly or indirectly in any of the 16 patients, regardless of the assay employed or the cell types/lineages genotyped (e.g., Fig 1b). In 2 patients with MYD88 L265P mutations, we found evidence for MYD88+ B-cells with discordant light chains by ddPCR (~0.1%) potentially implicating common lymphoid precursors (CLPs), but found no evidence for similar involvement of T-cells or monocytes. In 6 DLBCL patients experiencing relapse, tumor pairs profiled by CAPP-Seq (median depth 957) shared 93% of somatic mutations (75-100%, Fig 1c). Such pairs invariably shared clonal IgH VDJ rearrangements (4/4, 100%), thus implicating a common progenitor arising in later stages of B-cell development, not HSCs.
Conclusions: We find no evidence to implicate HSCs in the derivation of DLBCL. While formal demonstration of absence of pre-malignant HSCs in DLBCL would require overcoming practical and technical limitations (including number of available HSCs, sorting purity, and genotyping sensitivity), the pattern of shared somatic alterations at relapse makes this highly unlikely. We speculate that unlike lymphoid leukemias, the cell-of-origin for most DLBCLs reside later in B-lymphopoiesis, beyond CLPs.
(a) HSC sorting from BM by FACS (b) Allele frequencies of mutations found by CAPP-Seq in an examplary DLBCL case (x-axis) compared to the same variants in HSCs (y-axis). (c) Phylogenetic trees of DLBCL patients experiencing relapse (n=6) with tumor pairs sequenced by CAPP-Seq. Shown are the evolutionary distances between (i) germline and common inferrable progenitor (CIP) illustrating the fraction of shared mutations between tumor pairs, and (ii) CIP and both diagnostic (tumor 1) and relapse tumors (tumor 2) indicating unique mutations to each tumor.
(a) HSC sorting from BM by FACS (b) Allele frequencies of mutations found by CAPP-Seq in an examplary DLBCL case (x-axis) compared to the same variants in HSCs (y-axis). (c) Phylogenetic trees of DLBCL patients experiencing relapse (n=6) with tumor pairs sequenced by CAPP-Seq. Shown are the evolutionary distances between (i) germline and common inferrable progenitor (CIP) illustrating the fraction of shared mutations between tumor pairs, and (ii) CIP and both diagnostic (tumor 1) and relapse tumors (tumor 2) indicating unique mutations to each tumor.
Newman:Roche: Consultancy. Levy:Kite Pharma: Consultancy; Five Prime Therapeutics: Consultancy; Innate Pharma: Consultancy; Beigene: Consultancy; Corvus: Consultancy; Dynavax: Research Funding; Pharmacyclics: Research Funding. Diehn:Novartis: Consultancy; Quanticel Pharmaceuticals: Consultancy; Roche: Consultancy; Varian Medical Systems: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal