Abstract

Background: Acquired TTP is a potentially fatal syndrome, resulting from autoantibodies against ADAMTS13; however, ADAMTS13 deficiency or the presence of autoantibodies is not sufficient to cause disease or predict outcome. Infection or systemic inflammation often precedes the onset of acute TTP. We hypothesize that human neutrophil peptides (HNPs) 1-3, released from activated neutrophils or activation of complement, may be a trigger and a potential biomarker for acquired TTP; thus, we sought to determine the association between these biomarkers with in-hospital mortality during the acute setting.
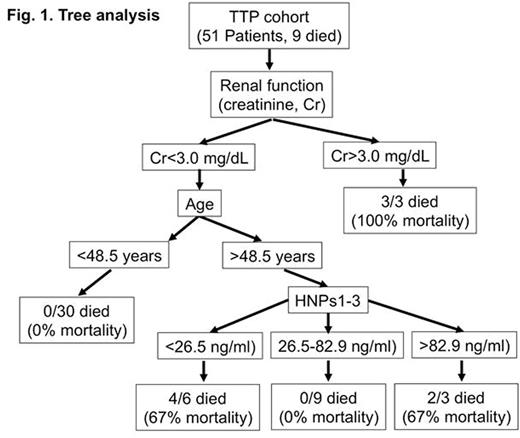
Methods: All patients admitted to our institution with the diagnosis of autoimmune TTP and ADAMTS13 level <10% between 2006 and 2015 were recruited to the study. Besides demographics and routine laboratory parameters, citrated plasma specimens were also analyzed for the levels of human neutrophil peptides (HNPs) 1-3 and complement activation markers (Bb, iC3b, C4d, and sC5b-9). These markers along with clinical and routine laboratory parameters were correlated with in-hospital mortality by univariate analysis. Decision tree analysis, a contemporary statistical method in data mining, was also used to identify parameters associated with mortality outcome.
Results: Fifty one patients (28 females, 23 males; mean age: 43.8 years; 35 patients with initial TTP episode) were eligible and had frozen plasma for laboratory analysis. On admission, prior to the initiation of therapeutic plasma exchange, the mean hematocrit (Hct), platelet count (Plt), and lactate dehydrogenase (LDH) were 24.3%, 19,130/mL, and 1,132.5 IU/L, respectively. The mean plasma levels of HNPs1-3, Bb, iC3b, C4d, and sC5b-9 were 47.1 ng/mL, 15.8 mg/mL, 3.3 mg/mL, 3.1 mg/mL, and 1.7 mg/mL, respectively. Nine patients died during hospitalization. Univariate analysis demonstrated that the patients who died tended to be older (p=0.01) and had relapsed disease (p=0.02). Other clinical variables (gender, ethnicity, neurologic symptoms) and laboratory variables (Hct, Plt, absolute neutrophil count [ANC], creatinine [Cr], LDH, HNPs1-3, and complement markers) were not statistically different between survivors and non-survivors; however, age, Cr, and LDH had high effect sizes (Cohen'd=0.81, 1.13, and 0.82) while ANC and HNPs had moderate effect sizes (Cohen'd=0.48 and 0.56). These results indicate that the differences have practical significance and would have reached statistical significance if the sample sizes were increased. Decision tree analysis (see Figure 1) further showed that all 3 TTP patients that had Cr ≥3 mg/dL died. Moreover, none of the 30 TTP patients younger than 48.5 years old died. Interestingly, in the group older than or equal to 48.5 years, the mortality rate was higher if the patients had HNPs <26.5 ng/dL or ≥82.9 ng/dL, as compared with those with HNPs between 26.5 and 82.9 ng/dL (67% vs. 0% mortality).
Conclusions: Mortality is increased in patients with acquired TTP if they are older (≥48.5 years), have worsened baseline renal function (Cr ≥3 mg/dL), or have baseline HNPs levels lower than 26.5 ng/dL or greater than or equal to 82.9 ng/dL. Complement activation markers and other baseline clinical and routine laboratory parameters were not different between survivors and non-survivors. Larger multicenter studies should be performed to confirm these findings, with attention to parameters with moderate to high effect sizes (i.e. age, Cr, LDH, ANC, and HNPs levels). Furthermore, basic science research is warranted to elucidate the role of HNPs in the pathogenesis of autoimmune TTP.
Zheng:Ablynx: Consultancy; Alexion: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal