Abstract

Background and objective: Blood loss associated with total lower-extremity joint arthroplasty (TJA) often results in postoperative anemia and need for red blood cell transfusions (RBCT).
We report the results of a quality improvement initiative to improve blood management and decrease transfusions in patients undergoing TJA in one tertiary hospital.
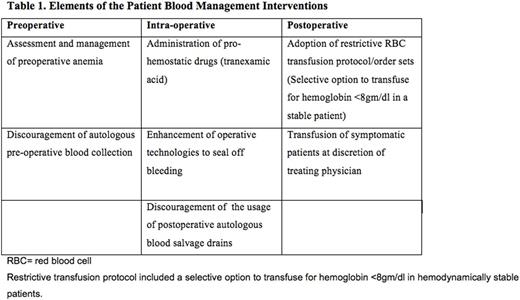
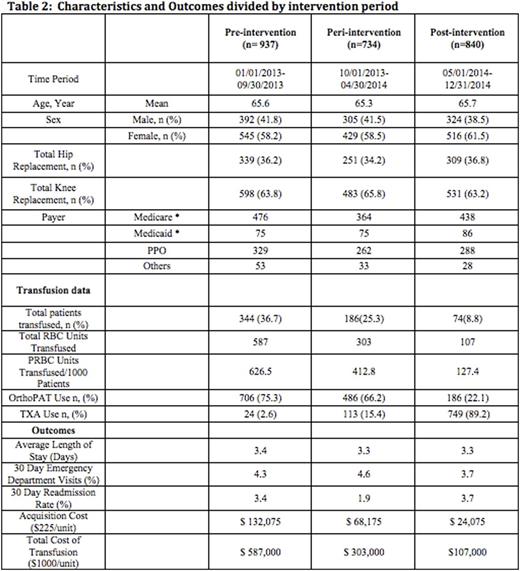
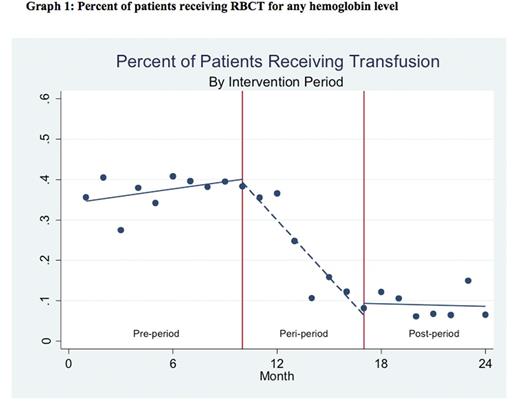
Methods: Pre and post analysis after the implementation of a multifaceted intervention which included preoperative assessment for anemia, use of tranexamic acid, discouragement of autologous pre-operative blood collection and institution of more restrictive RBCT protocols. The results were stratified into three periods: I - pre-interventional (01/01/2013 -09/30/2013); II - peri-interventional (10/01/2013 -04/30/2014); and III - post-interventional (05/01/2014 -12/31/2014). We used fractional logistic regression with robust standard errors and regression modeling was configured using a segmented, or "piecewise", approach in which slope coefficients in each period were estimated.
Results: During the study period 2511 patients underwent surgery. Compared with the pre-intervention period, the total number of RBC units transfused decreased from a total of 587 in the pre- to 107 in the post-intervention period (81.8% decrease). The percentage of patients receiving transfusion declined from 36.7% in pre-implementation period to 8.8% to post-intervention period. Depending upon the costing methodology used, annualized savings in RBC expenditure between time period 1 and 3 ranged from a low of $108,000 using the acquisition cost per unit (~$225/unit) to $480,000 when using activity based costing (~$1000/unit). Mean length of stay (days) and 30-day readmission rates remained stable during the study period.
Conclusions: A multidisciplinary approach with proactive involvement of all the interested parties can be successful and sustainable in reducing RBCT and its associated costs, in patients undergoing TJA.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal