Abstract
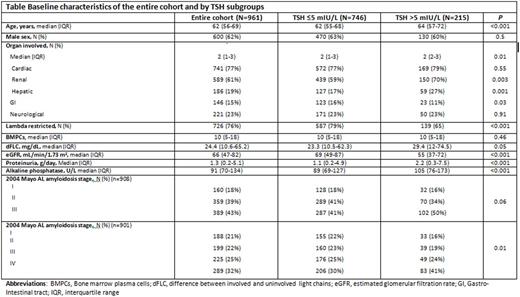
AL amyloidosis is a systemic disease with profound effects on organ function. However, despite the broad array of disease manifestations, the effect of AL amyloidosis on thyroid function is underreported. We explored the frequency of thyroid function abnormalities in 961 untreated AL amyloidosis patients seen in our clinic between 8/2005-8/2015, with emphasis on association with other organ involvement and tumor burden. Thyroid function was assessed using the thyroid stimulating hormone assay (TSH, normal range 0.3-5 mIU/L). If TSH was abnormal, measurement of free thyroxine (FT4) and thyroid peroxidase (TPO) antibodies was routinely performed. Patients' median age was 62 [interquartile range (IQR) 56-69], 62% were male (Table). The median number of organs involved was 2 (IQR 1-3), 29% of patients had more than 2 involved organs. Seventy-seven percent of patients had cardiac involvement, 61% renal, 23% peripheral/autonomic neuropathy, 19% hepatic and 15% gastro-intestinal (GI) involvement. The median difference between involved and uninvolved light chains (dFLC) was 24.4 [interquartile range 10.6-65.2 mg/dL]. The median TSH was 3 mIU/L (range 0.1-50.1); 22% had levels above the normal range and 8% of patients had TSH greater than 7.5 mIU/L. Baseline characteristics by TSH ≤5 mIU/L and TSH >5 mIU/L subgroups can be viewed in Table. Patients with renal or hepatic involvement had higher TSH values compared to no renal or no hepatic involvement (3.2 vs 2.6 and 2.8 vs 3.8, respectively; P<0.001 for both comparisons). There was a borderline significance for higher TSH in patients with >2 organ involvement compared to 1-2 affected organs (3.3 vs 2.8; P=0.05), with a strong trend for higher TSH for dFLC ≥18 mg/dL compared to dFLC<18 mg/dL (P=0.07). In patients with renal involvement, presence of proteinuria > 2 grams/day was associated with a higher likelihood of TSH >7.5 mIU/L (13% vs 5%; P=0.003). Free thyroxine (FT4) measurements were performed in 214 (22%) of patients with a median value of 1.1 ng/dL(range 0.3-72), 6% had levels below the lower limit (0.8 ng/dL). One-hundred and sixty five patients (17%) were screened for TPO antibodies, of which 16% (n=27) had an elevated titer. L-thyroxine (median dose 100 mcg/d, range 25-350 mcg/d) was already prescribed to 157 of the patients (16%) at their first visit, but duration of treatment prior to AL amyloidosis diagnosis could not be determined. Seventeen patients (1.5%) were prescribed amiodarone (median dose 200mg/d, range 100-400 mg/d), and although numbers were low, patients with amiodarone treatment had a TSH twice as high as patients without this treatment (6 vs 2.9 mIU/L, P=0.006). In conclusion, thyroid function abnormalities are frequent at the time of AL amyloidosis diagnosis and are influenced by type of organ involvement as well as disease burden assessed by dFLC and/or number of affected organs. Amiodarone, although infrequently used in this disease, can cause a profound disturbance in thyroid function among these patients.
Dispenzieri:Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; pfizer: Research Funding; Celgene: Research Funding; Alnylam: Research Funding; Prothena: Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees; Jannsen: Research Funding. Kumar:AbbVie: Research Funding; Array BioPharma: Consultancy, Research Funding; Glycomimetics: Consultancy; Celgene: Consultancy, Research Funding; Noxxon Pharma: Consultancy, Research Funding; Skyline: Honoraria, Membership on an entity's Board of Directors or advisory committees; Millennium: Consultancy, Research Funding; Onyx: Consultancy, Research Funding; Kesios: Consultancy; BMS: Consultancy; Sanofi: Consultancy, Research Funding; Janssen: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal