Abstract
Introduction:
The interaction of multiple myeloma (MM) cells with the bone marrow (BM) microenvironment is fundamental to MM pathogenesis. Cell adhesion-mediated drug resistance (CAM-DR) is regulated by adhesion receptors on MM cells such as CXCR4, CXCR7, CD49d and CD44. We and others have previously reported that CAM-DR towards drugs like bortezomib, pomalidomide or vorinostat may be dissolved by combining these novel agents with the CXCR4 inhibitor plerixafor. Different than expected, additional treatment with plerixafor in corresponding experiment however did not rescue the cytotoxic effects of the second generation proteasome inhibitor carfilzomib. We hypothesized that carfilzomib itself interferes with the CXCR4-CXCL12 axis in myeloma. Prior reports in AML and CLL indicate that PIM1-mediated CXCR4 phosphorylation at the position S339 is an essential step for CXCR4 recirculation to the cell surface and its function as CXCL12 receptor (Grundler et al. 2009, Decker et al. 2014). In this project, we therefore examined the effects of carfilzomib on the PIM1-CXCR4 axis as a not yet described, potentially class-distinct mechanism of action of this second generation proteasome inhibitor.
Methods:
U266, RPMI-8226, L363, MOLT-4, NCI-H929 and the stromal cell line M2-10B4 were utilized. Bortezomib (1, 10, 20, 50, 100nM), carfilzomib (20, 50, 100nM) and plerixafor (10, 50, 100μM) were used based on previous studies and are well comparable to clinically relevant doses. CXCL12 stimulation was performed with human recombinant CXCL12 (30nM). For combination studies, cells were preincubated with plerixafor (50µM). Viability was quantified by propidium iodide and annexinV-FITC using flow cytometry. For quantitative real-time PCR and Western blots, U266 monocultured cells were treated with a carfilzomib pulse (t=1h), were allowed to recover for 20 hours, starved for 4 hours and stimulated with CXCL12 for 15 minutes (n=4). PIM-1 mRNA transcript levels were assessed in U266 control vs. U266 treated with a carfilzomib pulse (100nM, t=1h) by qPCR. Data was analyzed according to the "delta-delta-CT method" based on the relative expression of PIM-1 vs. GAPDH. Results were normalized to the mean of the control samples.
Results:
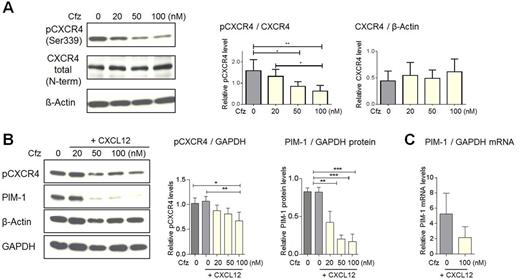
FACS analyses determined a substantial decrease of CD138 and CXCR4 surface expression in a dose-dependent manner after 1h carfilzomib treatment of U266 cells. Further assessment of downstream signaling revealed that carfilzomib treatment significantly reduces CXCR4 phosphorylation at S339 without changing total levels of CXCR4 (Figure A) or total levels of ERK or pERK (not shown), excluding a general inhibition of phosphorylation or protein synthesis by carfilzomib. Following the hypothesis that CXCR4 is potentially phosphorylated by PIM1 kinase, we assessed the impact of carfilzomib on PIM-1 protein levels: PIM-1 kinase protein was significantly reduced in a dose-dependent manner along with the levels of pCXCR4 in response to increasing doses of carfilzomib (0-100nM, Figure B). To further investigate a possible direct interference at the mRNA level, we evaluated PIM-1 mRNA levels after 1h carfilzomib, confirming substantially reduced PIM-1 RNA transcripts (Figure C). Different from carfilzomib and in line with prior observations (Shay et al. 2005), bortezomib was shown to increase protein levels of PIM-1 (data not shown). Side-by-side comparative assays of bortezomib vs. carfilzomib in terms of reduced CXCR4 expression, decreased CXCR4 phosphorylation and PIM-1 levels on mRNA and protein level are currently ongoing and will be presented at the meeting.
Conclusions:
Similar to previous reports on ixazomib reducing PIM-1 on protein and mRNA levels by inhibiting the tumor-suppressive microRNA miR33b (Tian et al. 2012), this work provides a potentially distinct mechanism of action of the second generation proteasome inhibitor carfilzomib on the PIM1-CXCR4 axis and identifies PIM-1 as a valid target to overcome CAM-DR in multiple myeloma.
Carfilzomib overcomes stroma protection due to PIM-1 kinase inhibition.
Engelhardt:Janssen: Research Funding; Amgen: Research Funding; MSD: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal