Abstract
Vaso-occlusive episodes (VOE), are considered a hallmark of sickle cell disease (SCD), and account for >90% of health care encounters for this patient population. Although an orphan disease (total number of patients in the US ~110,000), SCD has a huge medical-economic impact, with annual hospitalization costs of nearly $ 0.5 billion by 2004 figures, mostly for VOEs. The Cooperative Study of Sickle Cell Disease (CSSCD) was a large natural history study, carried in 23 Centers in the US, enrolling >3000 patients between 1977-93. An analysis of the frequency of VOEs in CSSCD showed that the majority of patients (80%) experienced 0-3 major pain crises/year; this was similar across all genotypes of the disease (SS, SC, Sβ0 thalassemia, Sβ+ thalassemia). Only a small minority (~5%) experienced ≥6 VOEs/year. Similar findings have been reported in subsequent, smaller studies, with 5-10% of SCD patients with frequent ED visits and hospitalizations. Hydroxyurea (HU), the only disease modifying agent approved for adults with SCD, results in a ~50% reduction in the frequency of VOEs and hospitalizations. Despite this, HU is underutilized in SCD. Recent NIH evidence based guidelines includes strong recommendations for HU therapy in the majority of SCD patients. Although 230 of the 650 adult SCD patients at our Center are prescribed HU, in a recent study we found that ~40% of these patients were non-adherent, based upon their own admission, and/or the lack of anticipated change in several laboratory parameters (Hb F, MCV, Hb, WBC, reticulocyte and platelet count). A minority of SCD patients followed at our Center have frequent ED visits and hospitalizations. We conducted a study analyzing demographic, clinical, laboratory and psycho-social characteristics of 25 patients with ≥6 ED visits and hospitalizations per year (high utilizers), and compared these with 9 patients (controls) who experienced ≤2 ED visits/hospitalizations (low utilizers). Data on gender, age, genotype, number of ED visits and hospitalizations, CBC, chemistry panel, Hb F, HU usage, opioid use (morphine equivalents), education level, employment, annual income and marital status were collected. All subjects were also administered a depression, anxiety and Health Locus of Control Questionnaire, and underwent quantitative sensory testing (QST) with three different modalities: pressure pain sensitivity with a hand held, computerized algometer (AlgoMed, Medoc, Israel), heat and cold sensitivity (Q-Sense, Medoc, Israel) and Von Frey monofilament testing for neuropathic pain.
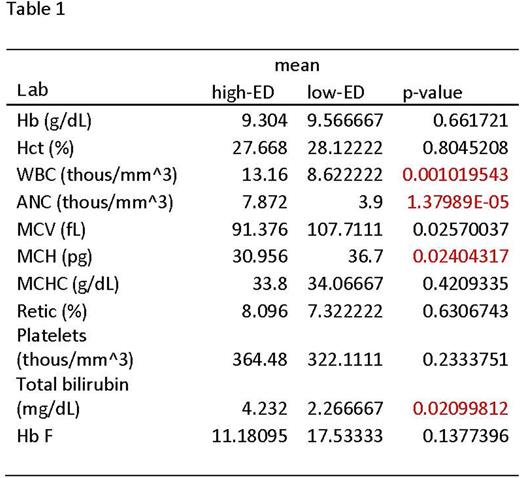
Of the 25 patients (13M, 12F), 19 were SS, 4 SC, 1 SD-Los Angeles and 1 Sdβ-thalassemia. The median age was 28 (range 21-49). In the low utilizer group (6M, 3F) all were SS with a median age of 39 (range 23-46). The average number of hospitalizations in the high utilizer group was 15.6/year (range 6-33), while in the low utilizer group it was 0.44/year. Annual opioid usage as mg morphine equivalents was significantly higher in the high utilizers (12125.7 mg vs 2423.1 mg, p=0.0048). 19/25 (76%) of high utilizers, and 7/9 (78%) of low utilizers were on HU. Laboratory data on both groups are shown in Table 1. High utilizers had significantly higher WBC, ANC, total bilirubin and lower MCV. Hb F was also lower in the high utilizers (11.8% vs 17.5%) although this did not reach significance. QST results showed significantly lower pressure pain threshold at ulna (224.4 KPa vs 338.9 KPa, p=0.04), and higher baseline sensitivity with von Frey monofilament (0.92 vs 0.33, p=0.056) in the high utilizer group. High utilizers also had a higher anxiety score (9.0 vs 4.6, p=0.039) and depression score (10.0 vs 6.0, p=0.051). While the low utilizers had higher education levels with more associate and bachelor degrees (p=0.009), there was no difference in household income. These data show that multiple factors contribute to high health care utilization in SCD; these include biologic (younger age, disease severity as indicated by higher WBC and ANC, bilirubin, opioid induced hyperalgesia, and poor adherence to HU) as well as psycho-social factors (higher anxiety and depression scores, lower educational status). A multi-disciplinary and multi-faceted approach, including a sound patient education and transition program, a concerted effort to increase adherence to HU therapy, and psycho-social as well as pharmacologic approaches to anxiety and depression will be required to address this complex problem.
Kutlar:Novartis Pharmaceuticals: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal