Abstract

Background: Children and adolescents with sickle cell disease (SCD) have high rates of healthcare utilization which peak around the age of transition from pediatric to adult care. Adherence to evidence based care, including regular clinic visits, annual transcranial doppler (TCD) studies, and hydroxyurea (HU) use, is often suboptimal in this population. Over the past 4 years we have used a registry and patient navigator to improve access to routine care for our patients with SCD. We hypothesized that increased access to clinic and higher rates of HU use would positively impact acute care utilization. The purpose of this study was to 1) assess adherence to clinic visits and TCD rates, 2) describe patterns of acute care utilization, and 3) analyze the association between response to HU and acute care utilization in our patient cohort.
Methods: We analyzed data on 208 unique patients with SCD between the ages of birth to 22 years of age who received care through the pediatric hematology program at BMC from April 2013 through March 2016. Demographics (age and genotype) and data on clinic visits, TCD screening, ED visits, inpatient stays, and HU use was obtained from the data ware house based on patients in our SCD registry. We calculated emergency department reliance (EDR), a ratio of clinic adherence relative to acute care utilization, for each patient.
TCD rates and HU use were analyzed for patients with HbSS genotype only. Patient were stratified into three HU categories; patients not prescribed HU, those prescribed HU with a HbF response of less than 15%, and those prescribed HU with a HbF response of at least 15%. A Kruskal-Wallis test was used to analyze differences in rates of acute care utilization between the HU groups, Wilcoxon rank-sum test was used to assess whether EDR differed by HbF category, and Spearman's rank correlation was used to test for an association between HbF and EDR.
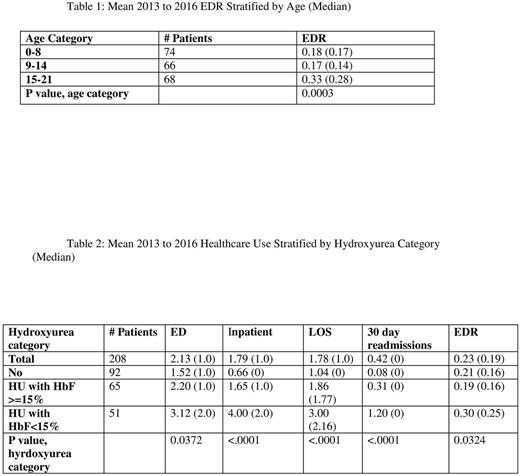
Results: On average over the three year period 78% of patients had two clinic visits per year, 85% of eligible patients were prescribed HU and 96% had annual TCD screening. Acute care utilization was higher among older patients, consistent with the existing literature. Patients in the oldest age bracket had the highest mean EDR at 0.33 (Table 1). Among patients prescribed HU, increased HbF% was associated with lower rates of acute care utilization among all measures analyzed (Table 2). There was also a statistically significant, inverse association between HbF percentage and EDR of -0.2183 (p=0.0275).
Conclusion: Through use of a SCD registry and patient navigator we have maintained adherence to biannual clinic visits, TCD screening, and HU uptake much higher than the rates reported in the literature. Our patients also had low rates of EDR at 0.23 which may reflect our clinic's accessibility. Increased levels of HbF, representing better adherence to HU, were associated with less acute care utilization, highlighting the importance of finding ways to increase adherence in our patient population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal