Abstract

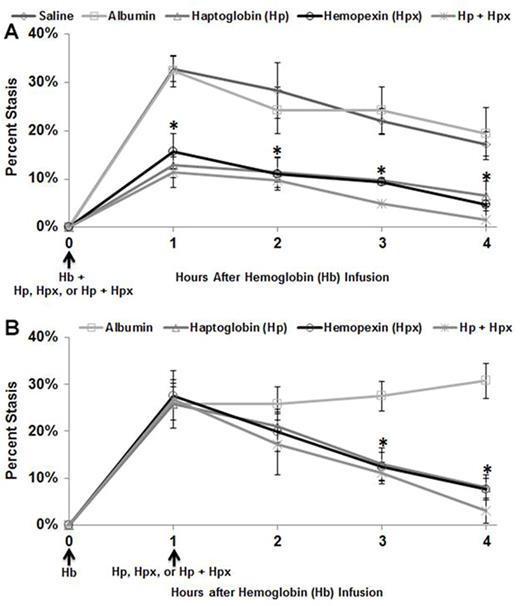
Free hemoglobin and hemin, released by red blood cells during intravascular hemolysis, promote vasculopathy, inflammation, thrombosis, and renal injury. Plasma haptoglobin and hemopexin tightly bind free hemoglobin and hemin, respectively, thwarting these clinical sequelae. In sickle cell disease (SCD), chronic hemolysis can deplete plasma haptoglobin and hemopexin in humans and mice. To explore mechanisms mediating this protection and provide a basis for supplementation in SCD patients, dorsal skin fold chambers were implanted onto Townes-SS mice and microvascular stasis (% non-flowing venules) was measured in response to a hemoglobin challenge. Human haptoglobin, hemopexin, or albumin was co-infused with hemoglobin or 1 hour after hemoglobin at equimolar concentrations. Sickle mice co-infused with hemoglobin/haptoglobin, hemoglobin/hemopexin or hemoglobin/haptoglobin/hemopexin had less stasis 1 to 4 hours after infusion, compared to albumin- and saline-treated mice (*p<0.01, Figure A). Haptoglobin, hemopexin, or haptoglobin/hemopexin given to Townes-SS mice 1 hour after hemoglobin, decreased stasis 2 and 3 hours after supplementation, while the venules of mice treated with albumin remained static (*p<.01, Figure B). Plasma hemoglobin and heme levels in Townes-SS mice were not different between treatment groups 3 and 4 hours after supplementation. Haptoglobin or hemopexin infusion increased hepatic Nrf2 and HO-1 and decreased pro-inflammatory NF-ĸB phospho-p65 expression relative to albumin 3 and 4 hours after supplementation (p<.05). The combination of haptoglobin/hemopexin was similar to either scavenger alone. Inhibition of the enhanced HO-1 activity afforded by haptoglobin or hemopexin with tin protoporphyrin blocked the stasis protection, confirming the critical cytoprotective role of HO-1. Haptoglobin and hemopexin, but not albumin, are cytoprotective in part by efficiently delivering heme to CD163 and CD91 and activating the Nrf2/HO-1 axis.
Belcher:CSL-Behring: Research Funding; Imara: Research Funding. Chen:Imara: Research Funding. Brinkman:CSL-Behring: Employment. Vercellotti:CSL-Behring: Research Funding; Imara: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal