Abstract

Introduction.
Minimal residual disease (MRD) is a powerful predictor of outcome in multiple myeloma (MM). We have previously demonstrated, in transplant eligible patients, that the level of MRD as a continuous variable independently predicts both PFS and OS, with approximately a one year median OS benefit per log depletion (J Clin Oncol 2013; 31:2540-7 and Blood 2015; 125:1932-5). The impact of MRD also appears to be independent of therapy received. There is more limited data on the applicability of MRD assessment in transplant ineligible patients, largely as a consequence of low rates of CR historically within this patient cohort.
Patients and Methods.
In this analysis we have assessed the impact of MRD on PFS amongst patients treated within the non-intensive arm of the NCRI Myeloma XI trial. Patients were randomised between thalidomide (CTDa) and lenalidomide (RCDa) based induction therapies with responding patients being subsequently randomised to maintenance with lenalidomide monotherapy, or no further therapy. Bone marrow aspirates were obtained at the end of induction and this analysis represents a subset of 297 patients (median age 74 years). MRD was assessed using flow cytometry (sensitivity 10-4) with a minimum of 500,000 cells evaluated with six-colour antibody combinations including CD138/CD38/CD45/CD19 with CD56/CD27 in all cases and CD81/CD117 in additional cases as required.
Results.
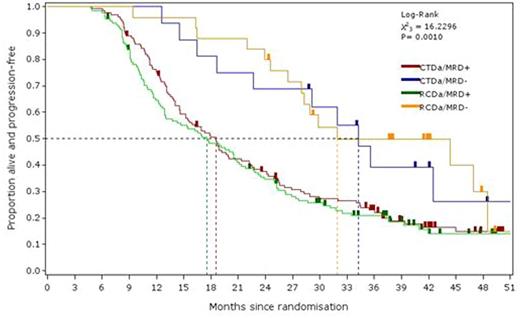
Overall MRD-negativity was demonstrated in 41/297 (13.8%). When considered according to induction therapy received 25/154 (16.0%) of patients randomized to RCDa were MRD-negative compared to 16/143 (10.8%) of those randomized to CTDa (p=0.24; Fisher's exact test). MRD-negativity was associated with a significant outcome advantage as the median PFS was 34 months versus 18 months for MRD-positive patients (p<0.0001, HR 0.44 [95% confidence interval (CI 0.29-0.67)]). This effect was noted in both RCDa (median PFS 17m v 32m; p=0.001, HR 0.41 [95%CI 0.23-0.69]) and CTDa (median PFS 19m v 34m; p=0.03, HR 0.49 [95%CI 0.26-0.95]). When the impact of MRD was assessed according to induction regimen the outcome of MRD-negative and MRD-positive patients was similar with both regimens (see figure). The impact of MRD was also assessed as a continuous variable across 5 logs of residual disease. Sequential improvements in outcome with each log reduction were demonstrable. Median PFS for the following disease levels; <0.01%, 0.01 - <0.1%, 0.1% - <1%, 1% - <10% and >/=10% were 34, 26, 16, 14 and 9 months respectively (p<0.0001). This pattern was demonstrable in both RCDa and CTDa treated patients (p<0.0001 for both). Multivariate analysis confirmed the independent predictive value of MRD both as a qualitative and continuous quantitative variable (p<0.0001 for both). In both instances achieving an immunofixation-negative CR was not a significant prognostic variable when included in the model with MRD.
Conclusions.
We would conclude that MRD is a powerful predictor of outcome in transplant ineligible patients and is a meaningful therapeutic goal in this patient group. In contrast to conventional CR it retains independent prognostic significance both as a quantitative and qualitative variable. This data further supports the role of MRD as a primary endpoint and surrogate marker for survival in future clinical trials.
Rawstron:Janssen: Research Funding; BD Biosciences: Other: Remuneration; Gilead: Consultancy, Honoraria, Research Funding; GlaxoSmithKline: Honoraria; Genzyme: Honoraria; AbbVie: Honoraria; Roche: Honoraria; Celegene: Honoraria. Pawlyn:Celgene: Consultancy, Honoraria, Other: Travel Support; Takeda Oncology: Consultancy. Davies:Janssen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Takeda: Consultancy, Honoraria. Kaiser:Amgen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Research Funding; Janssen: Honoraria; Takeda: Consultancy; Bristol-Myers Squibb: Consultancy, Other: Travel support; Chugai: Consultancy. Jones:Celgene: Honoraria, Research Funding. Cook:Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau; Glycomimetics: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Research Funding, Speakers Bureau; Amgen: Consultancy, Honoraria, Research Funding, Speakers Bureau; Bristol-Myers Squibb: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria, Speakers Bureau; Celgene: Consultancy, Honoraria, Research Funding, Speakers Bureau. Jenner:Janssen: Consultancy, Honoraria, Other: Travel support, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Other: Travel support; Takeda: Consultancy, Honoraria, Other: Travel support. Drayson:Abingdon Health: Equity Ownership, Membership on an entity's Board of Directors or advisory committees. Jackson:MSD: Consultancy, Honoraria, Speakers Bureau; Celgene: Consultancy, Honoraria, Other: Travel support, Research Funding, Speakers Bureau; Roche: Consultancy, Honoraria, Speakers Bureau; Amgen: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Speakers Bureau; Takeda: Consultancy, Honoraria, Other: Travel support, Research Funding, Speakers Bureau. Morgan:Celgene: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria; Bristol Meyers: Consultancy, Honoraria; Janssen: Research Funding; Univ of AR for Medical Sciences: Employment. Owen:Celgene: Consultancy, Honoraria, Research Funding; Takeda: Honoraria, Other: Travel support; Janssen: Consultancy, Other: Travel support.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal