Abstract
Introduction Hematopoietic stem cell transplantation from non-sibling donors remains the only curative option for severe aplastic anemia patients refractory to ATG/CsA immunosuppression. Although the results of MUD and haploidentical transplantation in SAA have improved significantly, graft-versus host disease (GVHD) remains a serious problem, associated with significant morbidity and mortality. We investigated the role of new method of graft processing - TCR alpha/beta depletion as a way to improve the results of MUD and haploidentical transplants in SAA.
Patients and methods Forty two patients with SAA were treated since November 2012 till February 2016. Median age at HSCT was 11(3-22) years, 27 male/15 female. All pts. were refractory/relapsed (36/6) after at least two courses of ATG/CsA, 3 pts. had concurrent severe hemolytic PNH. Time from diagnosis to transplant was 17(143-8,6)/15(99-5,5) months. Donors were unrelated volunteers in 32 cases, haploidentical parents in 10 cases. Preparative regimen included cyclophosphamide 100-150 mg/kg, fludarabine 150mg/kg, ATG and 2-6Gy thoraco-abdominal irradiation, in haplo transplants patients additionaly received thiophosphamide at 10mg/kg. Two patients recieved alemtuzumab instead of ATG because of anaphylaxis. Post-transplant GVHD prophylaxis included Tacro and Mtx on days +1, +3, +6. PBSC grafts were depleted of TCR alpha/beta cells and CD19 cells with CliniMACS device as recommended by the manufacturer. Patients received a median of 10(6,0-23) x106 CD34 per kg, 8(1-39) x104 TCR alpha/beta per kg.
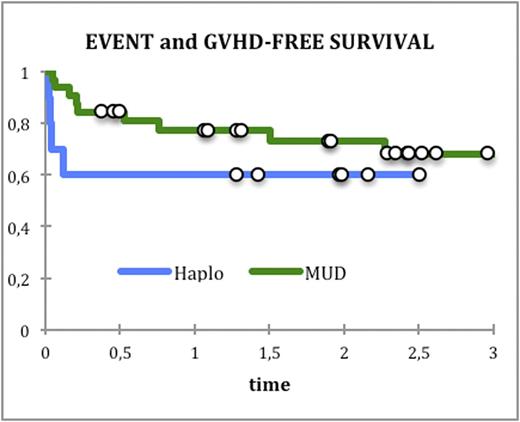
Results All patients engrafted with a median of 15 days for WBC and 13,5 days for platelets. In 4 patients after MUD transplantation secondary graft failure (rejection) developed, two of them were successfully retransplanted. Cumulative incidence of aGVHD 2-3 was 9% (95% CI: 3-27%) and 40%(95% CI: 18-85%) in MUD and haplo respectively, 90% patients with aGVHD had only skin involvement. No grade 4 aGVHD detected. Cumulative incidence of grade 3 aGVHD was 3%(95% CI: 0,5-21%) and 10%(95% CI: 2-64%) in MUD and haplo, respectively. Cumulative incidence of cGVHD was 12%(95% CI: 0,5-58%) and 30%(95% CI: 11-77%) in MUD and haplo respectively. A median follow up is 2 years. Seven patients died of viral infection - CMV (2 pts.), viral infection - CMV plus GVHD (2 pts.), microangiopathy (1 pt), 2 pts. died after second transplantation (1 - disseminated toxoplasmosis, 1 - ADV and CMV and GVHD). Event and GVHD-free survival is 73%(95% CI: 57-89%) and 60% (95% CI: 30-90%) in MUD and haplo respectively (pic.1)
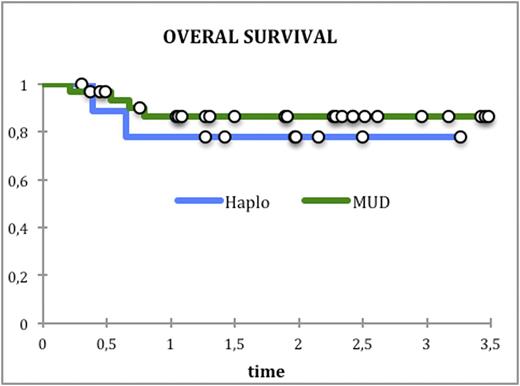
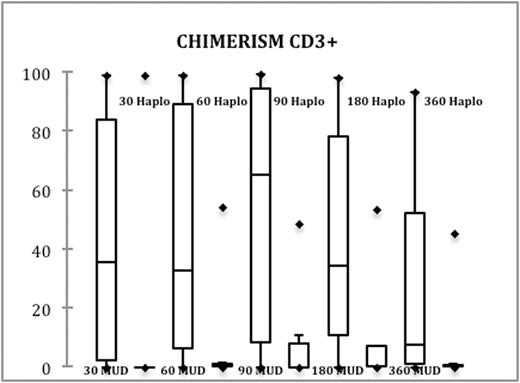
Overall survival is 86%(95% CI: 74-99%) and 78%(95% CI: 50-100%) respectively for MUD and haploidentical (pic.2). Prolonged stable mixed chimerism in T-cells was detected in recipients of MUD grafts in contrast to haploidentical grafts (pic/3).
Conclusion TCR alpha/beta depletion is a robust platform for allogeneic transplantation from MUD and haploidentical donors in severe aplastic anemia. Results should be further improved by additional measures to control viral infections and prevent rejection in MUD transplants.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal